Why Patients Ask How To Calm Overactive Nervous System
When a person sits in your exam room and asks how to calm overactive nervous system patterns, they are often describing a life where the accelerator stays pressed. They notice a quicker stress response when an email pings, a child cries, or traffic slows. Their nervous systems stay alert long after a stressful moment ends. Over time, that constant alertness drains reserve and narrows their capacity to adapt. The result is a nervous system overload that feels like being stuck in high gear.
Chiropractors see this every day. The solution begins with understanding the autonomic nervous system and the practical steps that activate recovery. Your role is to coach regulation techniques that bring the system back toward balance and to use objective analysis so you can show progress in a way that is obvious and motivating. With consistent guidance, patients learn how to calm the nervous system during the day and reset the nervous system at night, which supports better sleep, more stable energy, and improved nervous system performance.
The Autonomic Nervous System In Practice Terms
The autonomic nervous system is the behind-the-scenes regulator that keeps daily functions humming. It adjusts heart rate, coordinates breathing rhythm, supports digestion, and helps manage the body’s internal balance as the day unfolds. The autonomic nervous system is not a switch that is simply on or off. It is a dynamic interplay that adapts to your activity level, your environment, and your internal state.
Two branches share the work. The sympathetic nervous system is responsible for rapid mobilization. It sharpens attention, diverts blood flow to big muscles, and lifts alertness when the situation demands action. The parasympathetic nervous system helps you downshift and recover. It supports the relaxation response, stimulates digestive activity, and steadies heart rate variability so the body can refuel. In well-regulated nervous systems, the sympathetic and parasympathetic rise and fall throughout the day. You meet the challenge, then you recover.
Above this automatic network sits the central nervous system. The limbic system tags experiences as safe or threatening. That is why an intense conversation, a startling noise, or even a late-night worry can push the system toward high alert. When this pattern repeats, the nervous system may lean into sympathetic readiness by default. The practical goal in care is to regulate the nervous system so it can shift gears easily and return to a sense of calm after the response to stress has passed.
Recognizing The Signs Of Nervous System Dysregulation
Recognizing the signs of nervous system dysregulation begins with attentive listening. Patients describe tossing and turning, feeling wired when they want to sleep, or waking unrefreshed. They notice a heart rate that spikes with minor hassles. They report digestive changes even when no illness is present. They struggle to focus or feel unusually irritable. These are signs and symptoms that the system is activated more than it needs to be and that recovery is lagging.
- Elevated resting heart rate and shallow, upper-chest breathing.
- Trouble falling asleep or staying asleep, with morning fatigue.
- Digestive changes that reflect poor rest-and-digest activity.
- Persistent postural tension that lingers in quiet settings.
- Feelings of anxiety that do not match the situation.
Common causes of a dysregulated nervous pattern include poor sleep habits, schedule compression, constant screens, inconsistent meals, excess stimulants, and unresolved emotional triggers. Early exposure to antibiotics and other environmental toxins can add load. Chronic stress narrows adaptability over weeks and months. Your intake and your scans help patients see these patterns clearly, which is the first step in nervous system healing.
Learn more about INSiGHT scanning?
Fill this out and we’ll get in touch!
"*" indicates required fields
From Overdrive To Balance: A Clinician’s Aim
Think of the sympathetic system as the body’s emergency team. It is invaluable when you need to act. Problems emerge when the system kicks on too often or stays on too long. The clinical aim is not to turn off readiness. The aim is to improve nervous system balance so the body can move between states with ease. This is where you teach patients to activate the parasympathetic in small, repeatable ways during the day and before sleep.
Explain that nervous systems operate like energy budgets. When expenses exceed income for too many days, the account runs low. The work of regulation is like rebuilding savings. Each simple practice helps restore reserve. Over time, patients feel calmer, sleep better, and respond to daily challenges without the old spikes of arousal. This is resilience and calm you can measure.
Effective Ways To Calm And Regulate
The following regulation techniques are safe, clear, and teachable. Each strategy helps reduce stress load and supports the relaxation response. Encourage patients to listen to your body, move at a comfortable pace, and notice what helps them feel calm most reliably. These techniques can help across ages and fitness levels.
1) Breathing That Signals Safety
Deep breathing is a powerful, drug-free way to shift state. Slow, diaphragmatic breaths expand the belly on the inhale and lengthen the exhale. This pattern tells the brain there is no emergency. The physiological sigh is a simple version: take a deep inhale through the nose, add a short top-off sniff, then exhale slowly through the mouth. A few rounds can lower heart rate, quiet the stress response, and invite parasympathetic activity.
- Use 3 to 5 minutes before bed or after a stressful moment.
- Pair with a brief body scan to release postural tension.
- Coach patients to practice at the same times daily for consistency.
2) Gentle Movement With Rhythm
Walking, yoga, tai chi, or qi gong combine breath, rhythm, and awareness. These patterns help an overstimulated nervous system discharge excess arousal while bringing focus back to the present. Even ten minutes after meals supports digestion and state regulation. For desk workers, a brief mobility routine each afternoon steadies energy and prevents the late-day crash.
3) Sleep, Light, And Evening Routines
Regular sleep and wake times train circadian rhythm. Encourage dimming lights in the last hour of the evening and limiting screens. Recommend a short wind-down routine that includes slow breathing, gentle stretching, or reading. These habits tell the parasympathetic system it is time to restore, which steadies heart rate and promotes deeper sleep.
4) Nature, Social Connection, And Co-Regulation
Time outdoors and daylight exposure improve mood and help reduce stress. Encourage patients to schedule small doses of nature into their week. Co-regulation through trusted relationships also matters. A supportive conversation, a shared laugh, or a quiet meal can settle sensitive nervous systems and promote safety signals that the brain recognizes quickly.
5) Stimulant Review And Nutrition Steadiness
Caffeine and alcohol shift arousal in ways that can disturb sleep and amplify reactivity. Suggest reducing intake, especially late in the day. Encourage balanced meals with protein and fiber to steady energy across the day. Hydration supports physical health and cognition, which indirectly supports calmer states.
6) Deep Pressure And Heat As Comfort Inputs
Weighted blankets, vests, or pillows can provide deep pressure input that may help calm arousal. Many patients enjoy a warm bath or a localized heating pad in the evening. These inputs are optional and should be based on preference. The goal is to create a consistent routine that the nervous system associates with relaxation.
7) Bodywork And Emerging Self-Regulation Tools
Massage and self-massage can be excellent adjuncts for easing postural tension. Some patients explore tapping or gentle tremoring practices. Present these as options that may help calm the system. Remind patients that consistent, simple practices often produce the most reliable changes over time.
The Vagus Nerve And Practical Self-Coaching
The vagus nerve carries much of the parasympathetic signal between the brain and body. While there is no single switch to activate the vagus nerve on command, many of the simple practices above reliably stimulate the vagus nerve indirectly. Slow exhalations, humming or singing softly, gentle neck and jaw relaxation, and splash-cold water routines can nudge the system toward recovery. These are not cure-alls. They are small levers that, when repeated, improve how the nervous system acts across the day.
Coach patients to adopt a tiny protocol they can repeat at predictable times. For example, three physiological sighs, a thirty-second neck and shoulder release, and a short walk to the window for daylight. The details are less important than the rhythm. Consistency builds familiarity. Familiarity builds safety. Safety supports nervous system regulation.
How Chiropractic Fits: Adjustments Plus Measurable Coaching
Adjustments aim to ease neurological interference and restore motion through spinal regions so the system can adapt more efficiently. Many patients describe less reactivity and better sleep as they progress, which reflects improved regulation rather than the removal of stress itself. Your clinical expertise and your ability to coach simple daily practices are essential. This is where objective analysis adds clarity for you and confidence for the patient.
Explain that nervous system healing happens as the body learns to respond, then return to baseline more quickly. Healing is not a straight line. It is common for traits to fluctuate as loads change across the week. With scheduled rechecks and clear comparisons, you can demonstrate progress even when daily life is demanding.
The INSiGHT Tie-In: Turning Calm Into Something You Can See
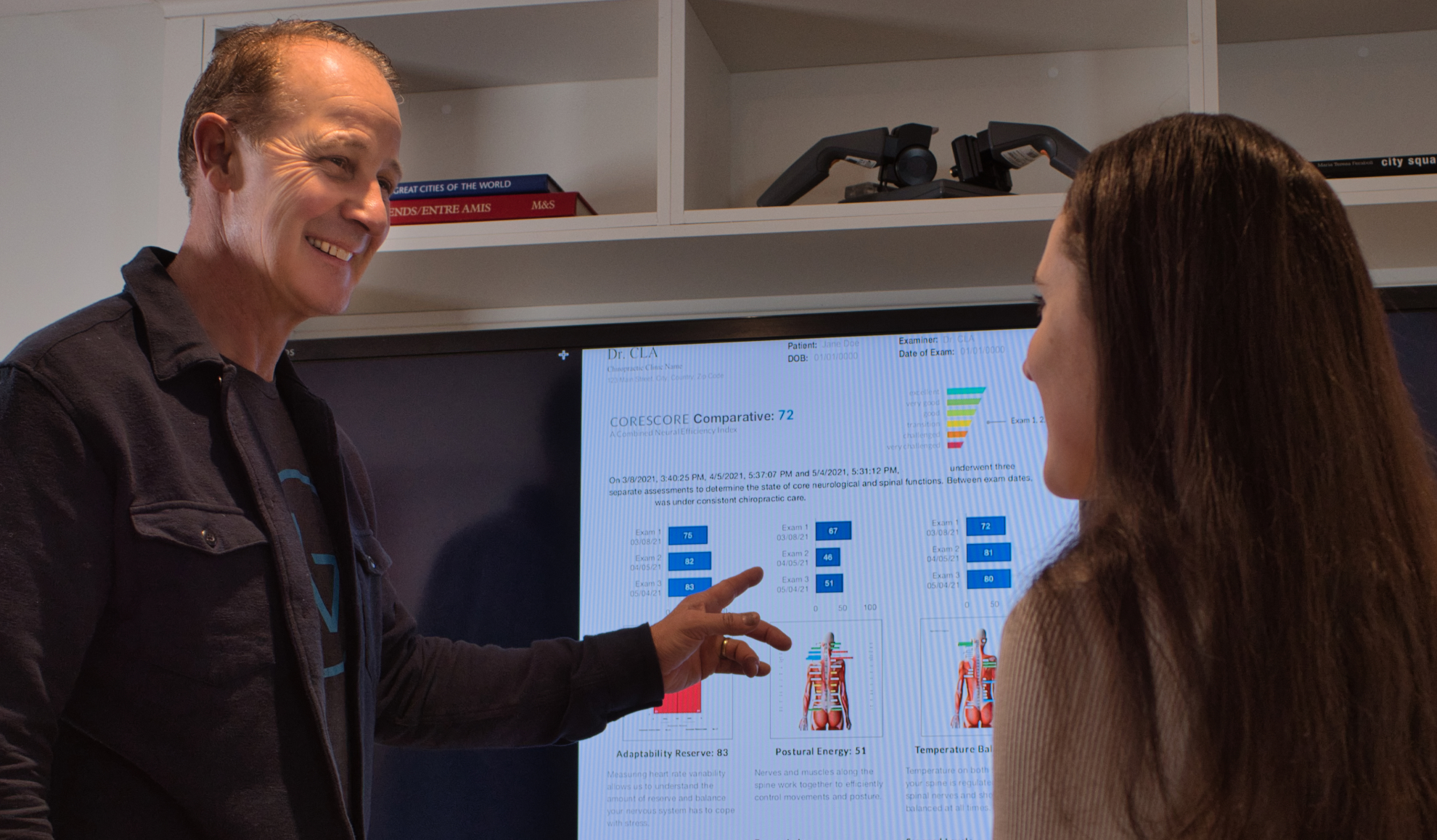
Neurological scanning shifts the conversation from guesswork to clarity. INSiGHT technology collects objective data and INSiGHT software translates it into color-coded scan views that patients grasp instantly. This is not about new buzzwords. It is about giving your care plan a measurable anchor and providing proof your care is making a difference.
neuroPULSE HRV And The Rainbow Graph
Heart rate variability analysis shows how the autonomic balance and overall activity look in real time. The Rainbow Graph makes sympathetic versus parasympathetic trends obvious, and it helps you track reserve as patients adopt simple regulation techniques. You can identify when the sympathetic nervous system is activated too often and whether parasympathetic activity is strengthening as routines take hold.
neuroTHERMAL For Neurological Distress Patterns
Thermal analysis highlights segmental and global patterns related to neurological distress. You can run rolling or segmental scans in under a minute and compare changes pre and post adjustment across visits. These views help patients see how their nervous system’s patterns are shifting, even before subjective traits fully stabilize.
neuroCORE sEMG For Symmetry And Fatigue
sEMG highlights asymmetry and recruitment patterns that correlate with postural tension and fatigue. As regulation improves, patterns often appear more efficient and symmetrical. This is not a promise of instant results. It is a way to document incremental improvements and align expectations with what the data shows.
Most important, remember that INSiGHT does not generate care plans. It generates objective exam data and reports. You, the chiropractor, interpret these findings and use them with your clinical expertise to design the patient’s care plan and set the cadence for re-exams.
A Simple Daily Micro-Routine You Can Teach This Week
- One minute of breathing: three to five rounds of a physiological sigh or slow diaphragmatic cycles.
- One minute of movement: gentle spinal mobility or a short hallway walk, focusing on relaxed shoulders.
- One minute of stillness: sit comfortably, soften the eyes, and notice the quieting sensation as heart rate settles.
Encourage patients to repeat this three-minute reset in the morning, mid-afternoon, and before bed. Attach the routine to cues they already have, such as brewing tea or closing the laptop. When the routine becomes automatic, the sympathetic and parasympathetic nervous systems shift more easily. Over time, the nervous system is balanced more often, which patients feel as steadier energy and clearer focus.
FAQ: Practical Questions Patients Ask
Is an overactive nervous system permanent?
No. Nervous systems learn. With consistent coaching, simple practices, and your care plan, the system learns to shift from high alert back to calm more efficiently.
Can breathing and movement really change my heart rate?
Yes. Slow breathing and gentle movement influence autonomic balance. They are effective techniques for guiding the relaxation response and improving daily adaptability.
How will I know I am improving?
Your traits will fluctuate less. Falling asleep becomes easier. Mornings feel steadier. INSiGHT scan comparisons make these changes visible, which keeps motivation high.
What if my system is sensitive?
Start small. Two minutes of slow breathing and a short walk is enough. Build gradually. The key is consistency, not intensity.
Could nervous system damage cause my symptoms?
Severe injuries and illnesses can affect regulation. Most patients presenting for wellness-oriented care are dealing with load and recovery imbalance rather than damage. Scans, exams, and your clinical judgment guide appropriate referrals when needed.
Making The Nervous System The Focus Of Your Practice
Your patients do not need perfect routines to feel better. They need simple tools, steady coaching, and objective feedback. Use INSiGHT scanning at baseline and rechecks. Teach a three-minute reset. Encourage gentle movement, consistent sleep, and time outdoors. Help them tune stimulants and meals so energy steadies. Encourage them to manage stress with small steps they will actually repeat. Over time, nervous systems that once felt stuck begin to shift. People notice they can meet the day and still settle at night. That is the work. That is how to calm overactive nervous system patterns in a way that lasts.