By Dr. Christopher Kent
As chiropractic approaches its centennial, it is appropriate to consider the direction our profession should take in the 21st century. Sociologist Wardwell wrote that chiropractic should become a “limited medical specialty” such as dentistry, optometry or podiatry, which does not challenge the theoretical basis of allopathic medicine. [1] Nelson has proposed that chiropractic be limited to a neuromusculoskeletal specialty. [2] Both authors suggest that our direction be determined by the public’s perception of the role of the profession.
The folly of such thinking is eloquently refuted by medical anthropologist Morinis.
“Only the chiropractic philosophy significantly distinguishes the chiropractic practitioner. And yet the philosophy is kept hidden away. It has done so in fear of being labelled quackery and this was undoubtedly a good strategy to follow at one time. The public knows next to nothing of chiropractic philosophy of healing and its mechanisms: If hospitals offer spinal manipulation, a chiropractor offers nothing else. This distortion of the chiropractic tradition can only be overcome by a reevaluation of the place of theory in chiropractic…Dispossessed of its philosophy, chiropractic is dispossessed of its uniqueness, and perhaps its future.” [3]
Korr admonished the osteopathic profession to hold fast to its principles: “There are misapprehensions about the source of your strength. Your profession appears to believe that its strength is to be found more in the stamps of approval by self-appointed magistrates of medicine…As a result, you often act as though you believed your strength is to be nurtured by mimicry, by cloaks of protective coloration, by compromise of principles, by organized compliance, by appeasement, and by adaptation to what is prescribed for you by organizations of another profession…Recent events loudly proclaim the futility of this approach.” [4]
It is ironic that Korr’s words of three decades ago are applicable to chiropractic today. His sentiments echo B.J. Palmer’s commitment to preserving the “big idea.” Korr wrote, “It is much too big and important an idea to be entrusted to those whose only concern with the idea is with how well or how poorly that idea — or one of its suitably diluted, distorted, corrupted and conventional sounding versions — serves the instrument, that is, the doctor and the profession. For them (the profession) is not an idea — much less a big idea — to be advanced on behalf of mankind. For them it is but a commodity to be sold — in whatever guise it will sell, quickly and in large volume, and with gratifying aggrandizement of the agent. I think we need, in some way, to re-infuse into the profession an appreciation of the immensity of the idea, of the profession’s responsibility to it, and of the vast opportunities to serve it.” [5]
It is significant that the first chiropractic patient, and many early patients of D.D. Palmer, did not present with back pain as a chief complaint. Most chiropractors know that D.D. Palmer reported his first chiropractic patient was relieved of deafness following a chiropractic adjustment. Fewer know that another early patient suffered from “heart trouble.”
According to D.D., “Shortly after this relief from deafness, I had a case of heart trouble which was not improving. I examined the spine and found a displaced vertebrae pressing against the nerves which innervate the heart. I adjusted the vertebra and gave immediate relief — nothing ‘accidental’ or ‘crude’ about this. Then I began to reason that if two diseases, so dissimilar as deafness and heart trouble, came from impingement, a pressure on nerves, were not other diseases due to a similar cause?” [6]
Although this physiologic explanation is overly simplistic by today’s standards, it demonstrated that D.D. understood the breadth and potential of his discovery.
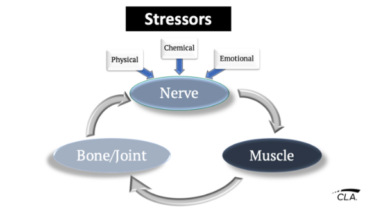
Today, a barrier to accepting the responsibility of educating the public on the role of the vertebral subluxation in pathogenesis is the misconception that there is no scientific basis for the chiropractic management of visceral, infectious, and endocrine disorders. A comprehensive review of the neurobiologic mechanisms associated with the subluxation is beyond the scope of this column. However, a brief overview of the facilitation model should offer sufficient evidence to dispel the notion that spinal subluxations are not capable of causing visceral dysfunction.
Korr proposed a model in which facilitation of sympathetic pathways leads to “high sympathetic tone.” Such facilitation, described as being associated with “lesioned” segments of the spinal cord, results in increased impulse traffic to viscera and blood vessels. According to Korr, “High sympathetic tone may alter organ and tissue responses to hormones, infectious agents, and blood components. It alters cellular metabolism and may eventually lead to serious pathologic changes.” [7]
Van Buskirk has proposed an update to the Korr model. In this model, nociceptors are postulated to be the primary receptors causing dysafferentation and resulting in high sympathetic tone. [8] Sato has offered experimental evidence which supports this model. Mechanical pressure applied to rat spines caused alterations in blood pressure, pulse rate, renal and adrenal sympathetic nerve activity.[9] The reader is referred to the review works addressing these and other relevant mechanisms. [10,11,12,13,14]
The acid test, of course, takes place in the clinic. Regardless of the elegance of a theoretical construct, it becomes an historical footnote if it fails in the real world. How do chiropractic and similar techniques fare clinically? The refereed literature in recent years has attracted papers dealing with case reports, theoretical models, and controlled studies related to non-musculoskeletal disorders. A small sampling follows.
Eye problems
Gilman and Bergstrand published a case report involving an elderly male with traumatic vision loss. Optometric and ophthalmologic examination revealed that no conventional treatment was appropriate. The lost vision returned following chiropractic care. The authors stated, “Behavioral optometrists have often been interested in the work of chiropractors and the resulting vision changes.” [15]
Schutte, Tesse and Jamison did a retrospective review of 12 children with esophoria, and concluded that such patients may respond to cervical spine adjustments. [16]
Changjiang et al reported on 114 cases of patients with cervical spondylosis who had associated visual disorders. Visual improvement was noted following “manipulative treatment” in 83% of these cases. Furthermore, of the 54 cases followed up for a minimum of six months, 91% showed a stable therapeutic effect. Cases of blind eyes regaining vision were included in the report. [17]
Gorman published a case report where a 62-year-old male with a one-week history of monocular visual defect experienced dramatic visual improvement after a week of “spinal manipulation.” Gorman stated, “Spinal manipulation can affect the function of the optic nerve in some patients presumably by increasing vascular perfusion.” [18]
Ulcers
Pikalov and Kharin compared the results of “spinal manipulative therapy” with traditional medical care in patients with endoscopically confirmed ulcer disease. Both groups received the same dietary regimen. Weekly endoscopic exams were performed. The group receiving spine care experienced pain relief earlier than the medical group. Clinical remission was observed an average of 10 days earlier in the SMT group than the medical group. [19]
Dysmenorrhea
Kokjohn et al studied the effect of “spinal manipulation” on pain and prostaglandin levels in women with primary dysmenorrhea. 45 subjects were included in the study. 24 were assigned to the experimental group, and 21 to the control group. The controls received a “sham” manipulation. The authors found that immediately after treatment, the perception of pain and the level of menstrual distress were significantly reduced. It was suggested that further studies be performed over a longer time frame. [20]
Infantile colic
A prospective, uncontrolled study of 316 infants with infantile colic showed a satisfactory result in 94% of cases receiving chiropractic care. The results occurred within two weeks. (21) Other authors have offered case reports of results obtained in patients with colic. [22,23]
Conclusions
Incomplete and superficial as this overview is, it is my hope that it will expand the vision of those who feel that chiropractic is a limited musculoskeletal specialty. Some might suggest that in the absence of large, multicenter controlled clinical trials, no claims of clinical utility should be made. To those who are critical of case studies and uncontrolled observations, it may be instructive to look at the level of evidence available for interventions generally accepted by the public and the medical profession.
According to David Eddy, former professor of health policy and management at Duke University, “Only about 15% of medical interventions are supported by solid scientific evidence. This is partly because only 1% of the articles in medical journals are scientifically sound and partly because many treatments have never been assessed at all.” [24]
Even more chilling is the deplorable safety record of allopathic medicine. According to a 1991 study by the Harvard Medical Practice Study Group in Cambridge, 80,000 persons die every year — one every seven minutes — as a result of negligence in hospitals. This makes medical malpractice the third leading cause of preventable death in the United States.[25] Despite the paucity of evidence supporting efficacy, and the plethora of evidence supporting risk, allopathic medicine stands as the de facto standard.
It is irrational to demand a more burdensome standard for chiropractic than allopathic medicine. Chiropractic has one of the most enviable safety records in the healing arts. Furthermore, it boasts a 100-year track record of helping patients with a variety of health problems. As a profession, we must now decide if we are going to permit an incomplete, aberrated perception of chiropractic to prevail merely because it’s an “easy sell,” or accept the challenge of educating the public concerning the immense value of our distinctive approach to the restoration and maintenance of human health.
Will we lead the revolution in 21st century healthcare, or will we accept a grotesque caricature of what chiropractic really is? The stakes are high, but the potential rewards immeasurable.
References
1. Wardwell W: “The triumph of chiropractic — and the what?” Journal of Sociology and Social Welfare 1980 7(3):425.
2. Nelson C: “Chiropractic scope of practice.” JMPT 1993 16(7):488.
3. Morinis EA: “Theory and practice of chiropractic: an anthropological perspective.” JCCA 1980 24(3):118.
4. Korr IM: “The function of the osteopathic profession: a matter for decision.” Keynote address to 63rd annual convention of the American Osteopathic Association. July 13, 1959. Chicago, IL.
5. Korr IM: “What ‘osteopathy’ and ‘the osteopathic concept’ mean to me” (1962). The Collected Papers of Irvin M. Korr. American Academy of Osteopathy. Indianapolis, IN. 1979.
6. Palmer DD: “The Chiropractors Adjuster.” Portland Printing House. Portland, OR. 1910.
7. Korr IM: “The Andrew Taylor Still memorial lecture: research and practice — a century later.” J Am Osteopath Assoc 1974 73(5):362.
8. Van Buskirk RL: “Nociceptive reflexes and the somatic dysfunction: a model.” J Am Osteopath Assoc 1990 90(9):792.
9. Sato A: “The reflex effects of spinal somatic nerve stimulation on visceral function.” Proceedings of the scientific symposium of the World Chiropractic Congress. May 4-5, 1991. Toronto, Canada.
10. Lantz CA: “The vertebral subluxation complex.” International Review of Chiropractic. Sep/Oct 1989 pages 37-61.
11. Korr IM (ed): “The neurobiologic mechanisms in manipulative therapy.” Plenum Press. New York. 1978.
12. Leach RA: “The Chiropractic Theories.” Williams and Wilkins. Baltimore, MD. 1980.
13. Cauwenbergs P: “Vertebral subluxation and the anatomic relationships of the autonomic nervous system.” In Gatterman M (ed): “Foundations of Chiropractic Subluxation.” Mosby-Year Book, Inc. St. Louis, MO. 1995.
14. Wiles MR: “Visceral disorders related to the spine.” In Gatterman M(ed): “Chiropractic Management of Spine Related Disorders.” Williams and Wilkins. Baltimore, MD. 1990.
15. Gilman G, Bergstrand J: “Visual recovery following chiropractic intervention.” Journal of Behavioral Optometry 1990 1(3):3.
16. Schutte B, Teese H, Jamison J: “Chiropractic adjustments and esophoria: a retrospective study and theoretical discussion.” J Aust Chiro Assoc Dec 1989 19(4):126.
17. Changjiang I, Yici W, Wenquin L, et al: “Study on cervical visual disturbance and its manipulative treatment.” Journal of Traditional Chinese Medicine 1984 4:205.
18. Gorman RF: “The treatment of presumptive optic nerve ischemia by spinal manipulation.” JMPT 1995 18(3):172.
19. Pikalov AA, Kharin VV: “Use of spinal manipulative therapy in the treatment of duodenal ulcer: a pilot study.” JMPT 1994 17(5):310.
20. Kokjohn K, Schmid DM, Triano JJ, Brennan PC: “The effect of spinal manipulation on pain and prostaglandin levels in women with primary dysmenorrhea.” JMPT 1992 15(5):279.
21. Klougart N, Nilsson N, Jacobsen J: “Infantile colic treated by chiropractors: a prospective study of 316 cases.” JMPT 1989 12(4):281.
22. Hyman CA: “Chiropractic adjustments and infantile colic: a case study.” In Proceedings of the 4th National Conference on Chiropractic and Pediatrics. International Chiropractors Association. Arlington, VA. 1994.
23. Pluhar GR, Schobert PD: “Vertebral subluxation and colic: a case study.” Chiropractic: The Journal of Chiropractic Research and Clinical Investigation 1991 7(3):75.
24. Smith R: “Where is the wisdom? The poverty of medical evidence.” British Medical Journal 1991 303:798.
25. Dye M: “Silent danger of medical malpractice. Third leading cause of preventable deaths in U.S.” Public Citizen May/June 1994, page 10.