By Dr. Christopher Kent
Magnetic resonance imaging (MRI) enables clinicians to obtain clear images of the human body without ionizing radiation. In chiropractic practice, MR imaging demonstrates the potentially devastating effects of subluxation degeneration. Prompt detection and characterization of vertebral subluxations is imperative to the application of appropriate corrective procedures.
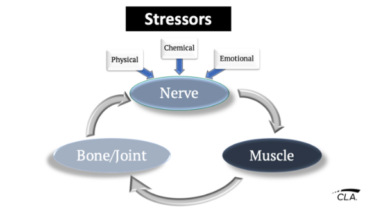
Subluxation degeneration is a process which may involve one or more pathophysiological mechanisms. The “common denominator” in these processes appears to be altered biomechanics, which results in local tissue pathology. These local changes may compromise neurological structures, causing abnormalities in peripheral structures. [111]
Modic et al [12] stated that MR imaging may be the appropriate first test for the evaluation of the cervical spine in degenerative conditions. The authors noted that disc herniation, canal stenosis, subluxation, and malalignment could be appreciated using MR imaging.
They concluded, “MRI can certainly replace plain film myelography for the overwhelming majority of situations…while the cost at first may seem prohibitive, the information that MRI is capable of providing in a noninvasive outpatient setting more than compensates for the expense.”
Karnaze et al [13] compared CT and MR findings in a retrospective study of 38 patients with suspected lesions of the cervical and thoracic spinal cord and canal. Nine of these patients demonstrated spondylosis. It was concluded that MR was equal or superior to CT myelography in depicting cases of cord enlargement, cord compression, and cord atrophy.
A paper by Koyanagi et al [14] reported that MR studies in three patients with spondylosis were able to directly show compression of the spinal cord. The authors noted that difficulty in detecting the abnormality at the thoracolumbar junction on plain radiographs often resulted in a delay in diagnosis.
Kulkarni et al [15] compared cervical spine images using cardiac gated spin echo images with those produced using gradient echo sequences in 41 patients. They concluded that cardiac gated spin echo sequences were better for depicting spinal cord lesions, while gradient echo sequences were superior in the diagnosis of degenerative disease in the cervical spine.
Takahashi et al [16] described the MR changes evident in 128 patients with compressive lesions of the cervical spinal canal. They found that high intensity lesions on T2 weighted images were generally observed in patients with constriction or narrowing of the spinal cord. This abnormality is thought to be due to myelomalacia or cord gliosis secondary to long standing cord compression. These devastating manifestations of subluxation degeneration were rarely appreciated by chiropractors prior to the availability of MR imaging.
In a retrospective study of 13 healthy subjects and 30 patients with degeneration of posterior spinal structures. Grenier et al [17] reported that sagittal MR images were useful in demonstrating hypertrophy of the ligamentum flava, facet degeneration, the degree of foraminal stenosis and measurement of the sagittal diameter of the spinal cord. Axial images facilitated the analysis of the facet joints, and permitted more accurate measurement of the thickness of the ligamentum flava and spinal cord diameter.
Batzdorf and Batzdorf [18] conducted an analysis of cervical spine curvature in 28 patients with cervical spondylosis. Plain films were used to evaluate spinal curves, and MR imaging was used to observe migration of the spinal cord. While there was no clear correlation between severity of myelopathy and altered curvature, it was observed that neck pain was most severe in patients with a reversal of the cervical curve.
The cerebrospinal fluid hypothesis of vertebral subluxation proposes that altered CSF dynamics result from alterations of sacral, vertebral, and cranial mobility. Klose et al [19] employed MR imaging to evaluate CSF oscillation. They reported that oscillation of the CSF within the cardiac cycle is superimposed by a directed movement. The authors stated the movement was cranial directed in the lateral cervical subarachnoid spaces, and caudal in the ventral subarachnoid spaces. The use of this technology to evaluate the effects of subluxation on CSF circulation holds promise.
In summary, the literature supports the use of MR imaging for the detection and characterization of the following manifestations of subluxation degeneration:
1. Subluxation and malalignment.
2. Intervertebral disc desiccation and degeneration.
3. Osteophytosis.
4. Corrugation/hypertrophy of the ligamentum flava.
5. Spinal canal stenosis.
6. Foraminal stenosis.
7. Disc herniation.
8. Facet asymmetry.
9. Facet degeneration.
10. Altered cerebrospinal fluid dynamics.
11. Cord compression.
12. Gliosis and myelomalacia
13. Spinal cord atrophy.
Since the discovery of chiropractic, it has been stated that vertebral subluxations have a deleterious effect on human health. The vertebral subluxation is not a matter of “faith” or “belief.” Magnetic resonance imaging is one technology that may be used to demonstrate the effects of vertebral subluxations on osseous and soft tissue structures.
In an era when some chiropractors eschew traditional chiropractic philosophy and deny the existence of vertebral subluxations, MR imaging has the potential of demonstrating important manifestations of this clinical phenomenon.
References
1. Akeson WH, Woo SL, Taylor TK, Ghosh P, Bushell GR: “Biomechanics and biochemistry of the intervertebral discs.” Clin Orthop (122):133, 1977.
2. White AA, Johnson RM, Panjabi MM, Southwick WO: “Biomechanical analysis of clinical stability in the cervical spine.” Clin Orthop (109):85, 1975.
3. Vernon H: “Static and dynamic roentgenography in the diagnosis of degenerative disc disease: a review and comparative assessment.” JMPT 5(4):163, 1982.
4. Ressel OJ: “Disc regeneration: reversibility is possible in spinal osteoarthritis.” ICA Review 45(2):39, 1989.
5. Posner I, White AA, Edwards WT, Hayes WC: “A biomechanical analysis of the clinical stability of the lumbar and lumbosacral spine.” Spine 7:374, 1982.
6. Nachemson A: “Towards a better understanding of low back pain; a review of the mechanics of the lumbar disc.” Rheumatol Rehabil 14(3):129, 1975.
7. Flesia J: Renaissance A Psychoepistemological Basis for the New Renaissance Intellectual, Renaissance International, Colorado Springs, 1982.
8. Huelke DF, Nusholtz GS: “Cervical spine biomechanics: a review of the literature.” J Orthop Res 4(2):232, 1986.
9. Leach RA: “The Chiropractic Theories.” 2nd ed. Williams and Wilkins, Baltimore, 1986. P. 3548.
10. Reiter L: “Apophyseal joint functional anatomy and experimental findings a literature review.” Res Forum 1(2):49, 1985.
11. Bullough OG, BoachieAdjei O: “Atlas of Spinal Diseases.” Lippincott, Philadelphia, 1988. P. 7692.
12. Modic MT, Ross JS, Masaryk TJ: “Imaging of degenerative disease of the cervical spine.” Clin Orthop (239):109, 1989.
13. Karnaze MG, Gado MH, Sartor KJ, Hodges FJ 3d: “Comparison of MR and CT myelography in imaging the cervical and thoracic spine.” AJR 150(2):397, 1988.
14. Koyangi I, Isu T, Iwasaki Y, Akino M, et al: “Radiological diagnosis of chronic spinal cord compressive lesion at thoracolumbar junction.” No Shinkei Geka 16(11):1227, 1988.
15. Kulkarni MV, Narayana PA, McArdle CB, Yeakley JW, et al: “Cervical spine MR imaging using multislice gradient echo imaging: comparison with cardiac gated spin echo.” Magn Reson Imaging 6(5):517, 1988.
16. Takahashi M, Sakamoto Y, Miyawaki M, Bussaka H: “Increased MR signal intensity secondary to chronic cervical cord compression.” Neuroradiology 29(6):550, 1987.
17. Grenier N, Kressel HY, Scheibler ML, Grossman RI, Dalinka M: “Normal and degenerative posterior spinal structures: MR Imaging.” Radiology 165(2):517, 1987.
18. Batzdorf U, Batzdorf A: “Analysis of cervical spine curvature in patients with cervical spondylosis.” Neurosurgery 22(5): 827, 1988.
19. Klose U, Requardt H, Schroth G, Deimling M: “MR tomographic demonstration of liquor pulsation.” ROFO 147(3): 313, 1987.