There are doctors of chiropractic who employ physical therapy modalities in clinical practice. I’ve heard many reasons for doing so. Some feel that modalities help to relieve pain. Others profess to be “preparing” the patient for adjustment by relaxing the paraspinal muscles. A handful even admit to using modalities “for the money.”
Whether their objectives are clinical or financial, these doctors should realize that contemporary evidence indicates that physical modalities are no better than placebos for pain relief, and may actually lengthen the duration of an episode of back pain. It is ironic that D.C.s employing physical therapy modalities often have a musculoskeletal pain treatment orientation.
Van den Hoogen et al published the results of a study involving 269 patients. The objective of these investigators was to identify prognostic indicators of the duration of low back pain in general practice, and the occurrence of a relapse. It was concluded that receiving physical therapy was associated with a longer duration of low back pain.
The authors reported, “at every moment in time, patients receiving physical therapy had a 61% less chance to recover in the following week than patients not receiving physical therapy.” (1)
Clinical Guidelines for the Management of Acute Low Back Pain, produced by the Royal College of General Practitioners in Great Britain, address the appropriateness of physical agents and modalities.
The Guidelines state that, “Although commonly used for symptomatic relief, these passive modalities do not appear to have any effect on clinical outcomes.” The modalities listed in the Guidelines include ice, heat, short wave diathermy, massage, and ultrasound.
How about bed rest and traction? Bad news.
“Traction does not appear to be effective for low back pain or radiculopathy. … The evidence shows that bed rest with traction is ineffective. It adds the complications of immobilsation to the deleterious effects of bed rest.”
MUA enthusiasts take note: “There is no evidence that manipulation under general anesthesia is effective. It is associated with an increased risk of neurological damage.” (2)
The AHCPR Guideline for Acute Low Back Problems in Adults concurs: “The use of physical agents and modalities in the treatment of acute low back problems is of insufficiently proven benefit to justify their cost.
“…Only two studies evaluated physical agents and modalities in patients with acute low back pain. Neither found significant differences in self-rated pain relief or other outcome measures between patient groups receiving physical agents and modalities (including diathermy, ultrasound, flexion/extension exercises, massage, and electrotherapy) and groups receiving a placebo.” (3)
What about pain control? Aren’t all those TENS units being promoted to D.C.s working?
A study of 324 patients found no differences in outcomes in those receiving three different types of TENS and those given a sham TENS unit with indicator lights but no output. (4)
Isn’t ultrasound effective?
Gam and Johannsen reviewed 293 papers published since 1950 to assess the evidence of effect of ultrasound for musculoskeletal disorders. Serious methodological problems existed in many of the papers. However, in 13 cases data were presented in a way that made pooling possible. The conclusion: “None of the methods gave evidence that pain relief could be achieved by ultrasound treatment.” (5)
Another meta-analysis looked at 400 randomized clinical trials. Meta-analyses were performed for disorders of the back, neck, shoulder and knee. Results indicated that, “In general, the methodological quality of the studies appeared to be low, and the efficacy of physiotherapy was shown to be convincing for only a few indications and treatments.” (6)
A controlled study was performed comparing osteopathic manipulation and short-wave diathermy in the treatment of non-specific low back pain The placebo group, which received fake diathermy, did about as well as those receiving real diathermy or osteopathy. The authors stated, “Benefits obtained with osteopathy and short-wave diathermy in this study may have been achieved through a placebo effect.” (7)
In a study comparing drug therapy, conservative physiotherapy and manipulative physiotherapy, “Serial assessments of pain and spinal mobility showed similar response rates in all three treatment groups and no significant difference between therapies.” (8)
Before a bevy of “shake and bake” chiropractoids pelt me with testimonials concerning the miracles they’ve seen with physical therapy, please note that these studies do not, for the most part, assert that physical therapy may not be associated with a favorable clinical response. The point is that if PT didn’t make you worse, it was generally not significantly superior to a placebo.
Of course, the framers of the “Mercy” document, not about to let their political agenda be confused by the facts, chose to produce “consensus” guidelines rather than “evidence based” guidelines. As a consequence, physical therapy modalities received an “established” rating, the highest rating possible. Adjusting for non- musculoskeletal conditions didn’t fare nearly as well. It will be interesting to see if they change their self-defined concepts of reality when faced with data.
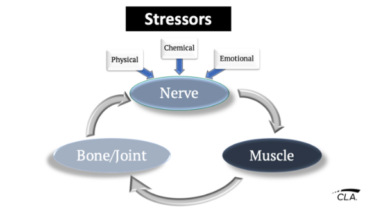
Yet, all of this begs the question, “Is pain control or disease treatment the objective of chiropractic care?” Certainly not! Chiropractic is concerned with the analysis and correction of vertebral subluxations. Doing so permits a less encumbered expression of the body’s innate potential. The correction of vertebral subluxation places the patient on a better physiologic path — one which permits the nervous system to select and execute the best course of action in a given circumstance.
In contrast, physical modalities seek to stimulate or inhibit, depending on the wishes of the doctor. Therefore, they override the body’s innate responses to the dynamics of the internal and external environment.
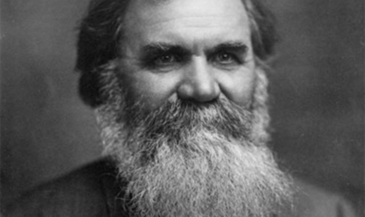
D.D. Palmer, the discoverer of chiropractic, wrote: “By adjusting, removing an impingement, we do not stimulate or inhibit; we only make conditions favorable for Innate to restore vital force to normal; normal energy produces normal heat and normal physiological metabolism.” (9)
B.J. Palmer, the developer of chiropractic, elaborated: “Chiropractic goes deeper than ‘treating backbones to stimulate or inhibit nerves;’ deeper than locating vertebral subluxations and adjusting them; deeper than locating specific cause of one dis-ease and correcting that specific to get sick people well — each being an empiric limitation or border beyond which our differing groups refuse to go. Chiropractic goes deep enough to want TO KNOW what makes vertebrates tick, including genus homo; why, how, when, where he ticks; for knowledge is power. Chiropractic has a NEW and greater insight into human existence to present.” (10)
References
1. van den Hoogen HJM, Koes BW, Deville W, et al: “The prognosis of low back pain in general practice.” Spine 1997;22(13):1515.
2. Clinical Guidelines for the Management of Acute Low Back Pain. Royal College of General Practitioners. September, 1996. Available at http://www.rcgp.org.uk
3. “Clinical Practice Guideline Number 14.” Acute Low Back Problems in Adults. Agency for Health Care Policy and Research. December 1994.
4. “No better than placebo. Another look at TENS units for low back pain.” Spine Letter 1997;4(5):2.
5. Gam AN, Johannsen F: “Ultrasound therapy in musculoskeletal disorders: a meta-analysis.” Pain 1995;63(1):85.
6. Beckerman H, Boulter LM, van der Heijden GJ, et al: “Efficacy of physiotherapy for musculoskeletal disorders: what can we learn from the research?” Br J Gen Pract 1993;43(367):73.
7. Gibson T, Grahame R, Harkness J, et al: “Controlled comparison of short-wave diathermy treatment with osteopathic treatment in non- specific low back pain.” The Lancet 1985;1(8440):1258.
8. Waterworth RF, Hunter IA: “An open study of diflunisal, conservative and manipulative therapy in the management of acute mechanical low back pain.” N Z Med J 1985;98(779):372.
9. Palmer DD: “Text-book of the Science, Art and Philosophy of Chiropractic.” Portland, OR. Portland Printing House Company (1910), p. 222.
10. Palmer BJ: “Answers.” Davenport, IA. Palmer School of Chiropractic (1952), p. 26.