Have you ever had that patient who keeps coming back with the same persistent headaches—the one who’s seen multiple specialists, tried every medication, and still can’t find lasting relief? You’re not alone.
Many of these chronic headache cases may actually be rooted in overlooked conditions like occipital neuralgia, which affects approximately 3.2% of patients, or cervicogenic headaches involving the greater occipital nerve, found in up to 4.1–20% of cases.
The frustration is real—both for you and your patients.
Most conventional approaches focus exclusively on symptom management, leaving patients caught in an endless cycle of temporary relief followed by recurring pain. Medications mask the problem while completely missing the underlying neurological dysfunction that drives these persistent symptoms.
Here’s the critical insight that’s often overlooked: the greater occipital nerve isn’t just another structure in the neck—it’s a primary communication pathway that reveals the true state of your patient’s neurological function.
This is where neurologically-focused care changes everything.
The Neuroanatomy of the Greater Occipital Nerve
The Greater Occipital Nerve (GON) originates as the medial branch of the dorsal ramus of the C2 spinal nerve, with some contribution from C3. Upon emerging, the nerve follows a complex journey through multiple tissue layers, creating several potential points of compression or irritation.
From its origin, the GON travels between the first and second cervical vertebrae, curving around the inferior oblique muscle of the head. It then pierces the semispinalis capitis muscle—a key point of potential entrapment—before continuing upward to penetrate the trapezius muscle.
The final portion of its journey involves piercing the aponeurotic attachment where the trapezius and sternocleidomastoid muscles meet near the superior nuchal line, approximately 3 cm below and 1.5 cm lateral to the external occipital protuberance.
This complex path creates multiple potential compression sites:
- Between the atlas (C1) and axis (C2) vertebrae—where a vertebral subluxation can directly impact nerve function
- At the inferior oblique muscle—where muscle tension can compress the nerve
- Through the semispinalis capitis muscle—a potential entrapment point
- At the trapezius aponeurotic attachment—which has been found to be a major entrapment site
- Along its superficial course—where it travels with the occipital artery in an intimate relationship
Once past these structures, the GON provides sensory innervation to the posterior scalp up to the vertex, the area above the ears, and the region over the parotid glands. What makes the GON particularly significant is its connection to the trigeminocervical complex—a group of neurons in the C2 dorsal horn that receive convergent input from both cervical and trigeminal nerves.
Understanding the Function and Vulnerability of the Greater Occipital Nerve
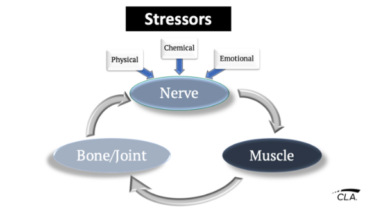
Subluxation plays a pivotal role in GON dysfunction. Remember that subluxation isn’t just about misalignment—it’s a complex neurological dysfunction characterized by altered positioning within the neurospinal system, abnormal tension or fixation, and neurological interference.
When subluxation affects the upper cervical spine, particularly at the C1-C2 level, it directly impacts the GON and can lead to occipital headaches.
Neurological interference disrupts the balance between nociception (the signaling of pain) and proprioception (the sense of body position). The primary factor that triggers neurological dysfunction is joint fixation and restricted movement, which affects proprioceptive input. Patients suffering from chronic musculoskeletal pain frequently demonstrate deficits in proprioception.
The GON’s intimate connection with the autonomic nervous system explains why patients with GON irritation often experience symptoms beyond simple pain—including dizziness, nausea, and visual disturbances. This could cause a shift toward sympathetic dominance—a state of “fight or flight” that affects everything from blood vessel tone to stress hormones.
Recognizing Greater Occipital Nerve Involvement in Patient Presentations
The classic presentation of occipital neuralgia includes a distinctive pattern of paroxysmal, shooting, or stabbing pain that originates at the base of the skull and radiates upward over the scalp. Patients often describe this pain as “electric,” “zapping,” or “shooting” in nature.
The hallmark signs and symptoms that suggest GON involvement include:
- Unilateral pain in the posterior scalp that may radiate toward the vertex or behind the eye
- Hypersensitivity of the scalp, sometimes so severe that patients report being unable to lay on a pillow or wash their hair
- Tenderness to palpation over the nerve pathway, particularly at the superior nuchal line
- Pain exacerbated by neck movement, especially extension and rotation
- Associated symptoms like dizziness, nausea, or visual disturbances due to autonomic involvement
- Numbness or paresthesia in the affected region
- Trigger points at specific compression sites along the nerve’s course
What conventional assessment misses is the underlying neurological dysfunction that INSiGHT scanning can reveal.
The Neurological Cascade
When the GON becomes dysfunctional, it initiates a neurological cascade through the trigeminocervical complex, which can lead to central sensitization. This fundamentally alters how the brain processes sensory information, lowering the threshold for pain perception and expanding the receptive field.
This explains why patients with occipital neuralgia often experience:
- Pain that radiates far beyond the GON’s anatomical distribution
- Hypersensitivity to stimuli that wouldn’t normally be painful (allodynia)
- Intensified pain response to normal painful stimuli (hyperalgesia)
- Expansion of the affected area over time
- Persistence of symptoms even after the initial irritation has been addressed
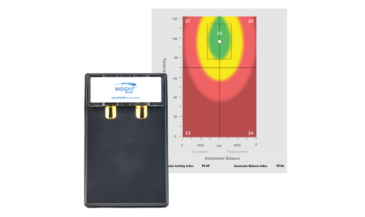
The autonomic component is equally significant. GON dysfunction typically shifts patients toward sympathetic dominance—a state of “fight or flight” that affects everything from blood vessel tone to stress hormones. This autonomic imbalance can be objectively measured using the neuroPULSE technology, which often shows decreased Heart Rate Variability in patients with chronic GON irritation.
Left untreated, this creates long-term changes through neuroplasticity that reinforce dysfunctional patterns, making the condition increasingly resistant to conventional treatments.
Comprehensive Assessment with INSiGHT Technology
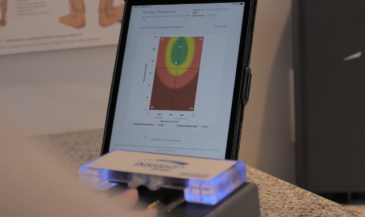
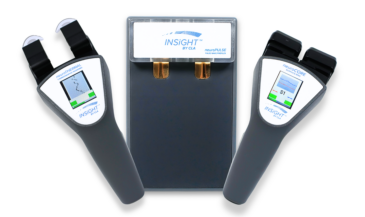
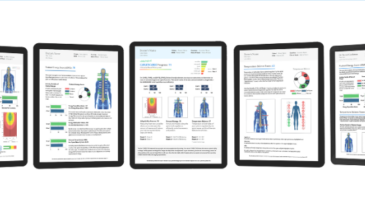
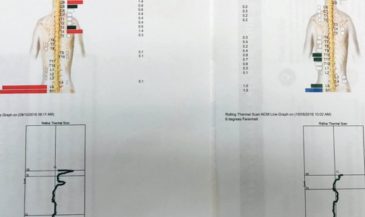
The INSiGHT neuroTECH suite provides a comprehensive neural profile through three complementary technologies:
- neuroCORE (sEMG) assesses paraspinal muscle activity, revealing patterns of tension, asymmetry, and dysponesis throughout the spine.
- neuroPULSE (HRV) measures Heart Rate Variability to assess autonomic balance and function and calculate adaptability and neurological control.
- neuroTHERMAL uses infrared scanning to detect temperature asymmetries along the spine, indicating spinal nerve distress.
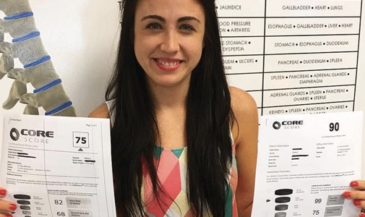
The integration of these technologies creates a CORESCORE—a comprehensive metric that quantifies neural efficiency and provides an objective baseline for measuring progress.
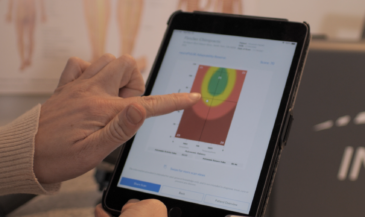
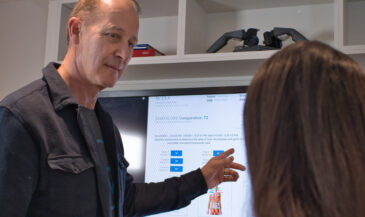
The visual nature of INSiGHT scans transforms patient education. When patients can see the patterns of muscle tension, autonomic imbalance, and thermal asymmetry, they gain a deeper understanding of their condition beyond “just a headache.”
Nervous System Focused Care Approach
A nervous system focused approach requires a shift from symptom management to addressing underlying neural patterns. The cornerstone is addressing upper cervical subluxation, guided by objective findings from INSiGHT scans.
Beyond structural correction, comprehensive care includes:
- Muscular component addressing: Reducing hypertonicity in the suboccipital muscles, semispinalis capitis, and trapezius.
- Neural inflammation reduction: Supporting the body’s natural anti-inflammatory processes through specific adjustments and lifestyle modifications.
- Autonomic balance restoration: Using Heart Rate Variability feedback to shift patients from sympathetic dominance toward balanced autonomic function. NeuroPULSE technology provides real-time feedback on this process.
- Proprioceptive retraining: Improving position sense and movement patterns in the upper cervical region.
We typically recommend scanning every 12 visits to document changes, following the “Four-scan sequence”—Initial, Progress, Comparative, and Continuation assessments. As we see improvements in the CORESCORE, patients can benefit far beyond headache relief.
Elevating Your Approach to Headache Care
Understanding the greater occipital nerve provides a powerful window into nervous system function. INSiGHT technology serves as the bridge between clinical science and practical application.
To implement this approach in your practice, start with a thorough neural assessment using INSiGHT technology. This will help you establish baseline measurements and create care plans that tackle all aspects of GON dysfunction, including structural, muscular, neural, and autonomic factors. Regularly reassess to track progress objectively, and use scan visualizations to educate patients about their neural function.
With our understanding of the greater occipital nerve and INSiGHT technology, we can now address the true source of these conditions—restoring neural function, balance, and adaptability in ways that transform not just headaches but overall health.
Your patients are searching for this level of care—care that looks deeper, measures objectively, and addresses causes rather than symptoms. By mastering the assessment and care of greater occipital nerve dysfunction, you position yourself as the expert they’ve been looking for.