Have you ever had a patient describe feeling lightheaded before unexpectedly fainting? While they may sound surprised or alarmed by the episode, you likely recognized the signs of a vasovagal response. You understand that this common reflex involves a sudden drop in heart rate and blood pressure, often triggered by specific stimuli like stress, pain, or prolonged standing, resulting in temporary loss of consciousness as the body’s protective mechanism.
More than 33% of people will experience a vasovagal episode in their lifetime. It’s the most common cause of syncope, affecting individuals across all age groups, with a particularly high prevalence in children and young adults.
Let’s be real. Most practitioners view these episodes primarily as cardiovascular events, focusing almost exclusively on the drop in blood pressure and heart rate. This limited perspective misses the deeper neurological story unfolding within your patient’s body.
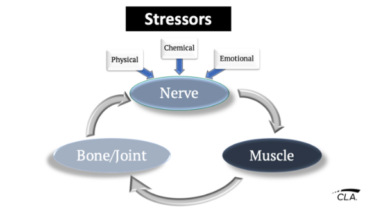
We understand that there’s a more profound story here, one that centers around autonomic function, neuroregulation, and the body’s adaptive responses to stress. The vasovagal response isn’t just a cardiovascular event; it’s a complex neurological cascade that reveals important information about your patient’s nervous system function.
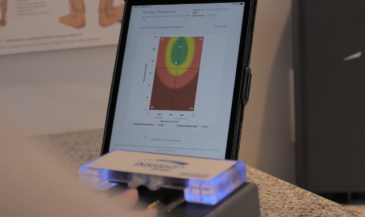
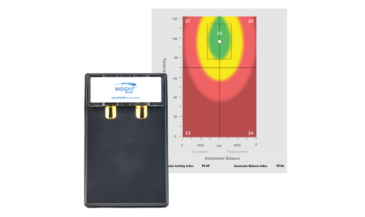
With INSiGHT scanning technology, we can finally measure and track these patterns objectively.
The Neurophysiological Foundation of Vasovagal Episodes
The vasovagal response has intrigued medical researchers for decades, with some theorizing it evolved as an adaptive mechanism to reduce blood loss during physical trauma. At the center of this response is the vagus nerve, the tenth cranial nerve, and the longest autonomic nerve in the human body, serving as the primary highway of the parasympathetic nervous system.
Understanding the neurological arc of a vasovagal episode requires examining both its afferent (sensory) and efferent (motor) pathways:
- Afferent Pathway: The cascade begins when specific triggers activate neural pathways that transmit signals to the brain.
- Central Processing: Within the brainstem centers, this sensory information leads to increased parasympathetic outflow and decreased sympathetic tone.
- Efferent Pathway: The resulting efferent signals travel through vagal pathways to the heart, causing bradycardia, while sympathetic withdrawal leads to peripheral vasodilation.
During a vasovagal episode, the autonomic balance shifts dramatically. As parasympathetic activity surges and sympathetic activity withdraws, the cardiovascular system undergoes a rapid reconfiguration: heart rate slows, blood vessels dilate, and blood pressure drops precipitously. When mean arterial pressure falls below the threshold for effective cerebral autoregulation, typically around 60 mmHg, cerebral perfusion becomes compromised, resulting in syncope.
What makes this particularly fascinating from our perspective is that INSiGHT scanning can detect these autonomic imbalances before they manifest as full episodes, giving us the opportunity for truly preventive care.
Technical Breakdown of the Vasovagal Response
To truly understand vasovagal attacks from a nervous system-focused perspective, we need to examine the entire episode as a sequence of distinct neurophysiological events.
The Trigger Phase
Common triggers include:
- Orthostatic stress: Prolonged standing causes blood pooling in the lower extremities.
- Emotional or pain responses: The sight of blood, fear, or acute pain activates central nervous system pathways.
- Environmental factors: Heat exposure can increase peripheral vasodilation.
- Physical strain: Activities like coughing, urination, or defecation can increase intrathoracic pressure.
- Dehydration or low blood volume: Reduced circulating volume sensitizes mechanoreceptors.
The Cascade Phase
Once triggered, the response unfolds through a precise sequence:
- Enhanced vagal tone: Parasympathetic outflow increases dramatically.
- Cardioinhibition: Vagal stimulation causes significant heart rate reduction.
- Sympathetic withdrawal: Simultaneous reduction in sympathetic activity causes widespread vasodilation.
- Peripheral blood pooling: Vasodilation increases peripheral vascular capacity.
- Reduced venous return: Blood pooling decreases central venous pressure.
- Decreased cardiac output: The combination of bradycardia and reduced filling lowers cardiac output.
- Cerebral hypoperfusion: When mean arterial pressure falls below the threshold for cerebral autoregulation, syncope results.
The Recovery Phase
Once the patient is horizontal, recovery begins almost immediately as gravity-assisted redistribution of blood volume improves venous return, baroreceptors sense improved central pressure, and cerebral perfusion is restored.
Recognizing Prodromal Signs
The prodromal symptoms that often precede syncope offer a crucial window for intervention:
- Dizziness and visual changes: Early signs of reduced cerebral perfusion
- Nausea: Vagal stimulation of the digestive tract
- Pallor and sweating: Sympathetic withdrawal affecting the skin
- Feeling of warmth: Peripheral vasodilation
From a neurological perspective, reflex syncope symptoms aren’t just warning signs, they’re direct manifestations of autonomic nervous system activity that can be objectively assessed through technologies like INSiGHT scanning.
Clinical Benefits of Neurological Assessment for Vasovagal Tendencies
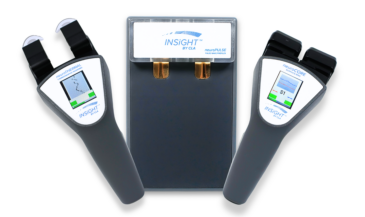
The neuroPULSE component of the INSiGHT technology provides valuable data by measuring Heart Rate Variability (HRV) to quantify the balance between sympathetic and parasympathetic activity. Individuals prone to vasovagal episodes may display:
- Altered sympathetic-parasympathetic balance at baseline
- Exaggerated autonomic responses to positional changes
- Reduced overall autonomic reserve capacity
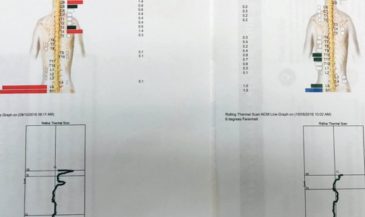
Surface electromyography (sEMG) through the neuroCORE scanner identifies areas of paraspinal muscle tension and inefficient energy expenditure in postural muscles, helping locate potential areas of subluxation affecting autonomic regulation.
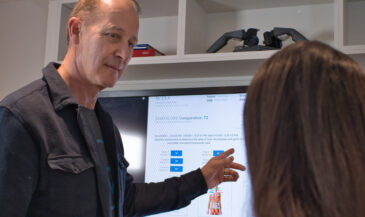
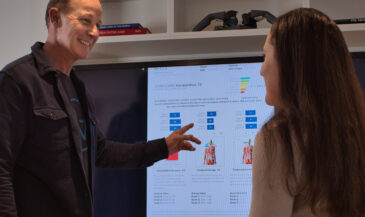
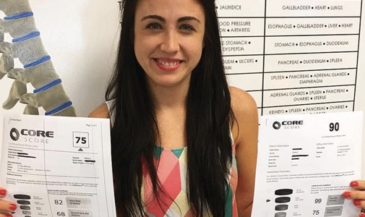
Perhaps most importantly, these technologies transform patient understanding and engagement. There’s a profound difference between telling a patient, “You have vasovagal syncope, so avoid triggers,” and showing them objective measurements of their autonomic function while explaining, “Here’s how your nervous system is currently operating, and here’s what we can do to help optimize its function.”
This objective data also documents improvement over time, providing tangible evidence of progress that reinforces the connection between neurological regulation and overall well-being.
Integrating Neurological Assessments
Implementing a nervous system-focused approach requires systematic assessment and clear communication:
Initial Assessment Protocol
- Comprehensive History: Dig deeper into autonomic function by asking about energy levels, temperature regulation, digestive function, sleep quality, stress resilience, and recovery capacity.
- INSiGHT Scanning: Complete a full assessment with particular attention to:
- HRV metrics (neuroPULSE) to assess autonomic balance
- sEMG (neuroCORE) to identify areas affecting neurological regulation
- Thermal scanning (neuroTHERMAL) to evaluate autonomic regulation of peripheral circulation
Beyond adjustments, equip your patients with effective prevention strategies:
- Physical countermeasures: Teach techniques like isometric contraction of the arms and legs and cross-legged muscle tensing to increase peripheral resistance.
- Hydration and electrolyte strategies: Recommend adequate water intake (typically 2-3 liters daily) and appropriate sodium consumption.
- Graduated orthostatic training: For particularly susceptible patients, suggest a program of gradually increased upright positioning.
Schedule regular reassessments using the INSiGHT scanning technology to document neurological improvement, guide refinements to your care approach, and provide patients with tangible evidence of progress.
The Horizon of Autonomic Assessment
The field of autonomic assessment is rapidly evolving, with promising implications for how we understand and address vasovagal tendencies. Advances in heart rate variability analysis are enhancing our ability to detect subtle autonomic imbalances before they manifest as clinical symptoms.
What’s especially encouraging is the growing recognition across healthcare disciplines of autonomic function’s importance. This creates opportunities for neurologically focused chiropractors to position themselves as leaders in this field, offering assessment capabilities that many other providers don’t have.
The connection between vertebral subluxation and autonomic function continues to be elucidated through research, strengthening the neurological foundation of chiropractic and expanding the potential benefits for patients with autonomic challenges.
Does Vasovagal Syncope Ever Go Away?
Vasovagal syncope can improve significantly or even resolve completely, particularly when the underlying nervous system dysfunction is addressed. Many people experience dramatic reductions in both the frequency and severity of episodes once spinal subluxation and autonomic imbalance are corrected through neurologically focused care.
While some individuals may retain a mild tendency toward these responses, the goal is restoring your nervous system’s ability to maintain stable cardiovascular regulation under stress. With proper care addressing the root neurological causes, many people find their episodes become so infrequent and mild that vasovagal syncope no longer impacts their daily life, demonstrating the remarkable healing capacity of a well-functioning nervous system.
Transforming Vasovagal Care Through Neurological Insight
By viewing vasovagal episodes through a neurological lens, we gain a deeper understanding and approach. Rather than seeing these episodes as random cardiovascular events to be endured, we recognize them as windows into autonomic function that can be objectively assessed and optimized.
The INSiGHT scanning technologies provide the objective metrics needed to make this shift from symptom management to neurological optimization. By measuring HRV, sEMG, and thermal patterns, we can identify the specific neurophysiological imbalances underlying vasovagal tendencies and track improvements.
Remember, what gets measured gets managed. Through objective neurological assessment with INSiGHT technology, we bring precision and clarity to what was previously vague and unpredictable, transforming both our approach to vasovagal episodes and our patient’s experience of care.
Now, that’s something to get excited about!