Hey Doc, have you ever had a patient describe episodes where they suddenly feel lightheaded, their vision starts to tunnel, and then they wake up on the floor? Maybe their family member mentions they saw some jerking movements and feared the worst. These moments can be incredibly concerning for everyone involved, but here’s what’s fascinating: these episodes often represent something entirely different from what they appear to be.
What’s even more encouraging? With the right neurological assessment tools, we can finally give patients real answers and measurable solutions.
Research shows that up to one in three people will experience a vasovagal syncope episode at some point in their lives. Yet, studies indicate that as many as 25% of individuals with cardiovascular syncope have been misdiagnosed with epilepsy, causing them to endure anticonvulsant medications with potentially serious side effects, all without addressing the true neural mechanism behind their episodes.
But what if these seizure-like events aren’t electrical misfirings in the brain at all? What if they represent something entirely different—a neurological miscommunication between the vagus nerve, heart, and brain that epilepsy approaches simply can’t detect or resolve?
Let’s explore the neurological reality behind vasovagal syncope seizures and why addressing underlying autonomic nervous system dysfunction may be the missing piece in resolving these frightening events.
What is Vasovagal Syncope?
The understanding of a vasovagal syncope seizure has evolved dramatically over the past several decades. What was once viewed as a primarily cardiovascular phenomenon is now recognized as a complex neuro-cardiovascular event with the autonomic nervous system at its core.
At the center of this neurological understanding is the vagus nerve—aptly named the “wandering nerve” as it extends from the brainstem through the neck and into the chest and abdomen.
Your left and right vagus nerves contain 75% of the nerve fibers in your parasympathetic nervous system. As the primary component of the parasympathetic nervous system, the vagus nerve serves as a critical regulator of numerous bodily functions:
- Heart rate control: The vagus nerve applies a “braking” effect on heart rate, slowing it down when activated
- Blood pressure regulation: Through its impact on heart rate and blood vessel tone
- Communication between brain and body: Transmitting signals in both directions.
- Inflammation modulation: Supporting immune regulation and stress response
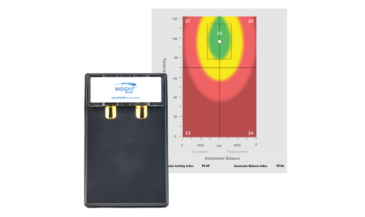
Heart Rate Variability (HRV) assessment, a core component of INSiGHT scanning technology, provides a window into this autonomic function.
Technical Breakdown of Vasovagal Seizures
Vasovagal seizures, more accurately termed “vasovagal syncope with convulsive activity,” represent a distinct neurophysiological event that differs significantly from epileptic seizures despite similar outward appearances.
The Neurophysiological Cascade
When a vasovagal syncope episode occurs, a complex sequence of neurological events unfolds:
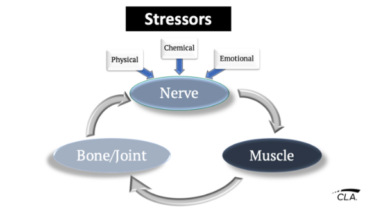
- Trigger activation: Exposure to a trigger—emotional distress, sight of blood, or other stressors—activates neural pathways
- Autonomic miscommunication: This sensory input triggers an abnormal autonomic response with an increased vagal tone
- Cardiovascular response: A parasympathetic surge can cause vasodilation and bradycardia
- Cerebral hypoperfusion: Drop in Blood pressure, reducing blood flow to the brain
- Loss of consciousness: Cerebral blood flow decreases below the threshold for consciousness
- Convulsive activity: As the brain experiences temporary hypoxia, seizure-like movements may occur
This entire sequence typically resolves as the person falls or is placed in a horizontal position, which restores cerebral blood flow and consciousness.
Distinguishing from Epileptic Seizures
Despite their outward similarities, vasovagal seizures have several distinguishing characteristics from epileptic seizures:
- Precipitating factors: Vasovagal syncope episodes typically have identifiable triggers
- Prodromal symptoms: Warning signs like lightheadedness, nausea, or visual changes often precede loss of consciousness
- Duration: Vasovagal convulsions are typically briefer (under 30 seconds)
- EEG findings: Show slowing of brain activity due to reduced blood flow rather than abnormal electrical discharges
- Response to medication: Do not respond to anticonvulsant therapies
Common Triggers
Numerous factors can trigger vasovagal syncope episodes:
- Emotional distress or anxiety
- The sight of blood or needles
- Prolonged standing, especially in warm environments
- Dehydration or decreased blood volume
- Pain, particularly abdominal or pelvic pain
- Straining during urination, defecation, or coughing
Susceptibility correlates strongly with autonomic nervous system regulation capacity, which can be measured through INSiGHT scanning technology.
Diagnostic Approach
The medical approach typically includes EEG, blood tests, ECG, tilt table testing, and brain imaging. While these tests have value in ruling out dangerous conditions, they often yield inconclusive results for vasovagal syncope episodes.
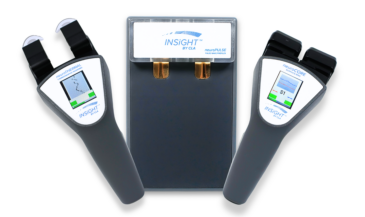
In contrast, our approach using INSiGHT scanning technology offers:
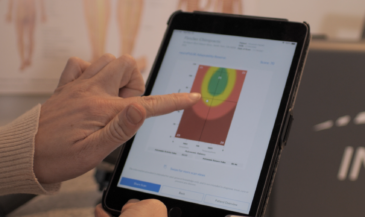
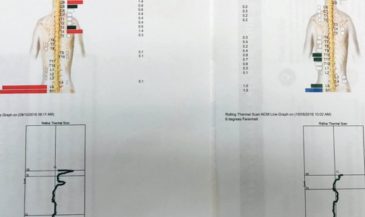
- Heart Rate Variability (HRV) assessment: Measures autonomic balance and vagal tone
- Surface Electromyography (sEMG): Evaluates neuromuscular patterns and tension
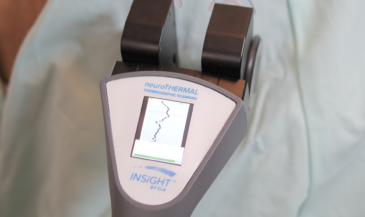
- Thermography: Assesses autonomic function through temperature regulation patterns
- Comprehensive neural efficiency calculation: Quantifies overall nervous system performance
This three dimensional, neurological assessment focuses on the nervous system’s underlying regulatory capacity rather than just identifying the presence or absence of specific conditions.
Clinical Benefits of Neurological Assessment
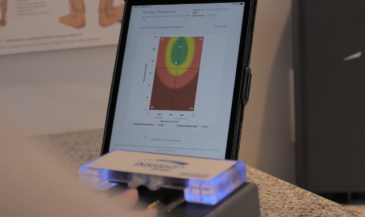
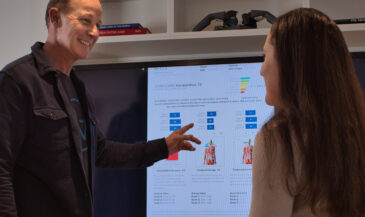
INSiGHT scanning technology offers unprecedented visibility into autonomic nervous system function. This technology transforms the assessment process from symptom-based guesswork to data-driven clinical decision-making.
The neuroPULSE component provides a detailed HRV assessment—a crucial metric for understanding vagal tone and autonomic balance. By measuring the subtle variations in time between heartbeats, HRV assessment quantifies regulatory capacity and identifies patients with compromised autonomic function before they experience vasovagal syncope episodes.
Surface Electromyography (sEMG) through the neuroCORE technology measures electrical activity in the paraspinal muscles, detecting patterns of tension, compensation, and dysponesis that often accompany autonomic dysregulation.
The neuroTHERMAL component completes the assessment triad by measuring skin temperature patterns along the spine, reflecting autonomic control of blood vessel dilation and constriction.
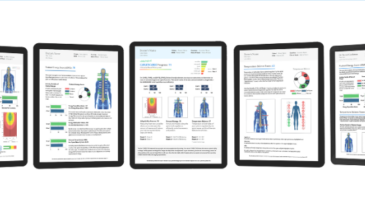
Together, these assessment tools create a comprehensive neural efficiency profile that serves multiple clinical purposes:
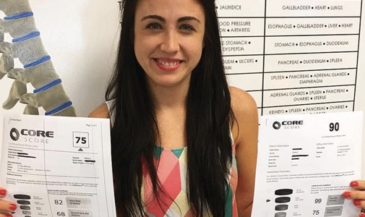
- Objective baseline documentation: Quantifying autonomic dysfunction before care begins
- Care plan customization: Targeting specific areas of neurological stress
- Progress validation: Demonstrating measurable improvements with care
- Patient education: Helping patients visualize and understand their nervous system function
Integrating Neurological Assessment
For patients with suspected or confirmed vasovagal syncope episodes, consider this comprehensive assessment sequence:
- Thorough history-taking: Document trigger patterns, prodromal symptoms, and recovery experiences
- Complete INSiGHT scanning: Perform baseline HRV, sEMG, and thermography assessments
- Trigger identification: Work with patients to identify their unique triggers
- Regular reassessment: Schedule follow-up scans to track progress objectively
Effective patient education transforms how patients understand their condition:
- Visual explanation: Use color-coded INSiGHT scan reports to help patients visualize their autonomic function
- Clarify mechanisms: Explain the “neural miscommunication” nature of vasovagal syncope episodes
- Focus on regulation: Emphasize that improving overall nervous system function creates resilience against triggers
- Progress demonstration: Show patients their improvement through comparative scans
Transform Your Approach to Vasovagal Care
The journey from confusion to clarity regarding vasovagal syncope seizures begins with a fundamental shift in perspective, recognizing these episodes as manifestations of autonomic nervous system dysregulation rather than isolated cardiovascular events or brain electrical abnormalities.
INSiGHT scanning technology provides the objective measurement tools needed to visualize and quantify autonomic function, transforming how practitioners approach these challenging cases.
By addressing the neural foundations of vasovagal syncope, you provide patients with something far more valuable than symptom management: you restore their confidence, independence, and quality of life. That transformation—from fear to freedom, from confusion to clarity—represents the true potential of care for vasovagal seizures.