If there’s one thing I’ve learned after decades in chiropractic, it’s that healthcare isn’t about best- guessing. It’s about listening and testing —listening not just to what a patient tells you, but what their body is quietly saying beneath the surface. And if you want to “listen in” on the nervous system, there’s no testing quite as illuminating as a surface EMG scan.
Let’s be honest: words like electromyography and neuromuscular conduction might sound like something out of a Chiropractic school lecture. But the way I see it, surface EMG scanning is one of the most down-to-earth, common-sense ways to check how the “wiring” of your spine and postural muscles is really working. Think of it like listening to the engine of a classic pickup truck—you want to know if it’s humming along or if something’s off. sEMG helps us do just that, only for the spinal nerves and muscle structures.
In this guide, I’ll walk you through what a surface EMG scan is, how it works, and why it’s become an essential part of the modern chiropractic approach—especially in neurologically focused care. I promise, by the end, you’ll see that this technology isn’t intimidating at all. In fact, it’s one of the friendliest tools in a chiropractic office.
What Is a Surface EMG Scan?
Let’s start at the beginning: surface EMG stands for surface electromyography. That’s a mouthful, but here’s what it means in plain English: It’s a safe, non-invasive scan that reads the electrical activity of the muscles along your spine—supported by peer-reviewed research. With this scan, we get a clear, real-time look at how your muscles are firing—where there’s balance, and where there might be trouble brewing beneath the surface. At CLA we take it one step further and ensure that the exam data is reproducible from scan to scan.
You might have heard of traditional needle EMG, which uses a small electrode inserted into the muscle. That’s mostly for hospitals and nerve specialists—not for our chiropractic practices. Surface EMG (the one we use) is much friendlier. We use the sophisticated wireless neuroCORE instrument which has incredible electronics operating in a handheld device.
So, what does a surface EMG scan actually measure? It picks up the electrical signals—what we call action potentials—that your nerves send to your muscles, telling them to contract, relax, or stabilize.Its incredibly “expensive” to manage gravity and so when a spine is out of balance or has compensated and its alignment over time, sEMG gives a clear picture of how neuromuscular energy is bein g spent to handle gravity. If those signals are clear, your spine’s functioning as it should.. If the signals look fuzzy or out of balance, that’s a clue: there is likely deeply embedded nerve interference or postural compensations, often before you ever feel a single ache. sEMG can detect these issues well before symptoms show up.
If you’ve ever had an EKG (or ECG) to check your heart, surface EMG is the spinal cousin to that test. It’s quick, clear, and it doesn’t hurt a bit. And for chiropractors who care about what’s happening beneath the surface, sEMG is a game-changer.
The Science and Simplicity of sEMG
Here’s where things get interesting—without getting complicated. Surface electromyography works by using sensors (those little electrodes) to pick up the electrical signals from the muscle fibers just below the skin. Each time your muscles contract, they send out a tiny jolt of electricity. The surface EMG scan measures this electrical activity and gives us a picture—almost like a weather map—of what’s going on along your spine.
Here’s what sEMG helps us detect:
- Muscle imbalance: Sometimes, one side of your spine is working harder than the other, often as a way to compensate for stress, spinal misalignment, or old injuries.
- Nerve interference: If your nerves aren’t sending clean signals, it’ll show up as abnormal patterns on the scan—often linked to vertebral subluxation. Research in JVSR supports this finding.
- Chronic tension or exhaustion: Even if you don’t feel pain, sEMG can reveal if certain muscles are overworked or underactive.
- Compensatory patterns: The body is smart—it adapts. But sometimes those adaptations aren’t efficient and can lead to trouble over time.
This isn’t just theory or a sales pitch. Published studies have shown that surface EMG is reliable and valid for detecting changes in muscle activity associated with spinal misalignment and neurological impairment. And it’s all done with no needles or radiation—just safe, repeatable care.
Why Surface EMG Matters in Neurologically Focused Chiropractic
If there’s a “secret sauce” to neurologically focused chiropractic, it’s being able to see and measure what’s going on with the nervous system—objectively. Surface EMG lets us do just that. It gives us a “stress map” of your spine: where the nerves are firing cleanly, and where there might be trouble brewing.
Here’s why sEMG is so vital:
- Posture is neurological. When posture is off, it’s rarely just about how you’re sitting or standing. It’s about how your nervous system is telling your muscles to work.
- Silent dysfunctions: Many problems start long before pain arrives. Surface EMG can detect abnormal patterns before symptoms ever appear.
- Objective progress: With sEMG, care plans aren’t based on guesswork. We can show you the data—where things are changing, and where more work is needed.
sEMG is essential for:
- Initial assessments: Establishing a baseline so we can measure improvement. (Source)
- Progress checks: Seeing how your nervous system is adapting, visit by visit.
- Personalized care: No two people are the same; your sEMG results help us create care that’s just for you.
The bottom line: In neurologically focused chiropractic, a surface EMG scan isn’t just a tool—it’s a necessity.
What to Expect: The Surface EMG Scan Experience
I always tell new patients: “This scan is so simple, you’ll wonder why every doctor doesn’t use it.” Here’s how it goes:
- Sensor placement: We use the neuroCORE instrument to detect the neuromuscular signals at 15 separate levels along your spine.
- Data collection: You’ll sit comfortably. The scan takes just two minutes, with no sensation at all.
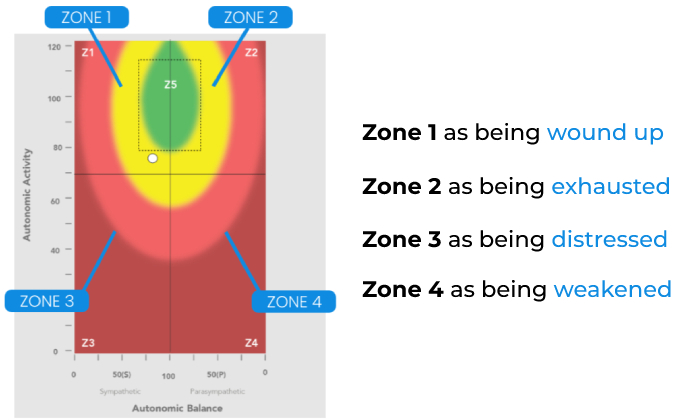
- Results in real time: The EMG system instantly transforms those electrical signals into a color-coded map. It’s like watching a weather radar, but for your spine.
This isn’t just for show. Seeing those patterns—the reds, yellows, and blues—makes it real for people. Suddenly, what’s been hiding beneath the surface becomes visible. It’s a powerful moment for many patients. Research shows that seeing sEMG results helps patients understand their neurological health and motivates engagement.
We use sEMG for more than the first visit. Over time, regular scans help track your body’s adaptation—whether you’re recovering from chronic low back pain, building resilience, or simply trying to stay ahead of neck pain and postural issues.
Frequently asked questions:
- Is it safe? Yes. There’s no risk, no pain, and it’s fine for kids, adults, and seniors. Sensors pick up signals and do not send any electrical current into the spine.
- How often do I need it? Usually at the start of care, and then during progress checks or when we’re re-evaluating your care plan.
- What does it show? sEMG measures muscle firing, balance, and stress patterns along your spine—making the invisible, visible.
Seeing Is Believing: Tracking Postural Health and Progress
One of my favorite things about the surface EMG scan is how it turns subtle, complex neurological data into something simple and visual. For patients, it’s not just numbers—it’s their health journey, mapped out in living color.
With each scan, we can:
- Compare before-and-after patterns, so you see progress as it happens.
- Highlight imbalances and compensation patterns, helping target care where it’s needed most.
- Catch small changes early, so nothing gets missed in your health plan.
This is especially important for folks dealing with ongoing issues—chronic pain, muscle fatigue, or even those subtle signs that something’s just not right. Surface EMG provides real feedback, in real time. It’s motivating, it’s transparent, and it puts you in the driver’s seat of your own care.
Bringing Surface EMG Into Clinical Practice
If you’re a fellow chiropractor or part of a care team, let me say this: Bringing surface EMG scanning into your workflow is one of the best decisions you can make for your patients and your practice culture.
Here’s how it fits into clinical practice:
- Baseline scans: Every new patient gets a surface EMG scan to set a reference point.
- Progress checks: Regular scans (every few weeks or months) show how well the nervous system is adapting to care.
- Adjusting care plans: Data from each scan helps us fine-tune strategies, making adjustments as targeted and effective as possible.
- Patient education: The scan visuals turn complex neurological concepts into something any patient can understand.
Over time, you’ll see better outcomes, more engaged patients, and a clinic culture that values transparency and excellence. That’s what we strive for at INSiGHT CLA—and what I hope for every chiropractor out there.
INSiGHT CLA and neuroTECH: Where Technology Meets Care
Let’s talk about the tools. At INSiGHT CLA, we take a lot of pride in designing technology that’s as user-friendly as it is advanced. Our neuroTECH suite—and especially the neuroCORE system—makes surface EMG scanning a breeze for any practice.
No complicated setups, no second-guessing sensor placement. The INSiGHT software (powered by Synapse) does the heavy lifting—translating signals into clear, colorful graphics you and your patients can understand. This isn’t just about technology; it’s about making care better, one scan at a time.
What really sets INSiGHT apart isn’t just the hardware. It’s our commitment to ongoing education, research, and supporting chiropractors who want to do things right. With INSiGHT, you get more than a machine—you join a community that’s shaping the future of neurologically focused chiropractic. Ongoing research and education back the use of sEMG in practice.
Want to dig deeper? Check out our full blog on tracking postural health with surface EMG scans here.
Looking Forward: The Future of Chiropractic Is Objective, Personal, and Bright
If you take away one thing from this article, let it be this: surface EMG scan is the tool that helps us “hear” the nervous system’s story, loud and clear. No more guesswork—just honest, objective insight into how the body is coping, adapting, and moving forward.
Whether you’re a seasoned doc or a new patient, integrating sEMG into your journey is one of the most powerful ways to build trust, track progress, and personalize care. And with tools like INSiGHT’s neuroCORE, every scan is another step toward a healthier, more resilient nervous system.
This isn’t just about technology. It’s about understanding people, respecting their stories, and meeting them where they are. That’s what we do at INSiGHT CLA. That’s what I believe chiropractic should be.
Frequently Asked Questions About sEMG
What is surface electromyography (sEMG) and how does it work?
Surface electromyography (sEMG) is a non-invasive technique used to measure the electrical activity of muscles through sensors touching the skin. It captures the action potentials generated by motor unit action potentials, providing insights into muscle contraction patterns and neuromuscular function. This technology is particularly useful in clinical settings for assessing muscle health and diagnosing conditions such as amyotrophic lateral sclerosis.
How is surface EMG useful in clinical evaluation?
The clinical utility of surface EMG lies in its ability to provide real-time feedback on neuromuscular activity, making it invaluable for the assessment of various neuromuscular disorders. For instance, surface electromyography improves the understanding of muscle response in patients with low back dysfunction and chronic pain conditions, allowing for better treatment planning and monitoring of rehabilitation progress.
What are the common applications of surface electromyography in the diagnosis?
Surface electromyography is widely used in the analysis of vertebral subluxations. It helps in evaluating the muscle fiber conduction velocity and identifying abnormalities in muscle activation patterns. Clinical studies have demonstrated its effectiveness in the assessment of the lumbar erector spinae providing critical information for patient management.
What are the benefits of using multi-channel surface EMG?
Using multi-channel surface EMG allows for a more comprehensive analysis of muscle activity across multiple sites. This approach enhances the reliability of surface EMG techniques by capturing a broader range of EMG measures, which can improve the understanding of muscle coordination and activation patterns during various tasks. It is particularly beneficial for research in electrodiagnostic medicine.
How does surface EMG contribute to understanding muscle contraction?
Surface EMG contributes to understanding muscle contraction by providing quantitative measures of EMG activity associated with different types of muscle contractions. This information can be vital in both research and clinical settings, helping to interpret the results of muscle performance and inform therapeutic interventions for conditions such as chronic pain and muscle dysfunction.
What role does surface EMG play in chronic pain assessment?
In chronic pain assessment, surface EMG plays a critical role by helping to identify dysfunctional muscle activation patterns that may contribute to pain. By analyzing the muscle response during specific movements, clinicians can tailor rehabilitation strategies and monitor outcomes based on the patient’s clinical status and response to treatment.
Can surface electromyography be used in research studies?
Yes, surface electromyography is frequently used in clinical studies and research to investigate neuromuscular function and the effects of various interventions. It provides valuable data on muscle activation and contraction patterns, which can be analyzed in studies published in journals such as the Journal of NeuroEngineering and Rehabilitation and the Journal of Clinical Neurophysiology.
What are the limitations of surface EMG?
While surface EMG is a powerful tool, it does have limitations. It may not capture deep muscle activity effectively, and factors such as electrode placement and skin condition can affect the reliability of results. Understanding these limitations is essential when interpreting surface electromyography studies, particularly in the context of complex conditions like amyotrophic lateral sclerosis.