Surface electromyography (sEMG) is more than just a reading of muscle activity. It’s a real-time analysis of how efficiently the motor nerves are directing energy to postural muscles along the spine. And when surface EMG is abnormal, it tells us something vital: the nervous system is working harder than it should—or not working enough—to maintain upright posture and spinal control.
So, what happens if surface EMG is abnormal?
It means the nervous system isn’t coordinating muscle tone properly. That can show up as postural fatigue, protective tension, poor adaptation, or early signs of neurological interference—often before symptoms even appear. In this article, we’ll explore what those abnormal EMG patterns really mean, why they appear, and how they shape care plans in practices that use INSiGHT’s advanced scanning technology.
If you’re ready to shift the conversation from posture to performance, let’s start with what EMG actually measures—and why it matters so much.
What Surface EMG Measures—and Why It Matters
Surface EMG (electromyography) is a non-invasive diagnostic test that evaluates how motor nerves interact with spinal postural muscles. Rather than analyzing symptoms of nerve or muscle dysfunction through physical exams alone, surface EMG measures the electrical activity that underlies muscle tone and coordination.
It’s important to clarify the difference between surface EMG and needle EMG. A traditional EMG test may involve a needle electrode inserted into the muscle to diagnose muscle disorder or nerve damage, often in hospital or medical center settings. This is typically done by a neurologist to identify nerve compression syndromes like carpal tunnel or neuropathy. These emg and nerve conduction studies can be uncomfortable and are diagnostic in nature.
By contrast, surface EMG uses surface electrodes placed on the surface of your skin, with no penetration. The electrical signals detected come from underlying nerve and muscle function, offering a view of postural efficiency and neurological distress.
Within the INSiGHT CLA suite, this technology is called neuroCORE. It records the electrical impulse through spinal motor nerves and translates this data into easy-to-understand scan views using the following core metrics:
- Total Energy Index: Measures overall energy use to maintain posture. Reference value = 100 for adults, 125 for children.
- Symmetry Score: Evaluates left/right neuromuscular balance.
- Pattern Score: Measures the top-to-bottom organization of postural muscle tone.
When EMG results are abnormal, chiropractors gain insight into inefficiency, overexertion, and compensation—all of which help guide neurologically focused care.
What Abnormal Surface EMG Results Actually Mean
When EMG results show abnormal patterns, it’s not a red flag for disease—it’s a signal of nerve dysfunction. These patterns reveal how the nervous system is coordinating (or failing to coordinate) muscle tone under gravitational load.
Abnormal EMG scans typically present as:
- Hypertonicity: Overactive firing due to spinal guarding or neurological interference.
- Hypotonicity: Low tone areas where the nervous system isn’t recruiting muscle properly.
- Asymmetry: One side working harder, indicating nerve or muscle imbalance and compensation.
These aren’t isolated “muscle problems.” They’re signs of abnormal electrical activity along the nerve roots, often caused by vertebral subluxation, nerve compression, or prolonged sympathetic overdrive. A patient may appear symptom-free, but still show significant postural inefficiencies on their surface electromyography test.
Rather than waiting for muscle weakness, muscle pain, or loss of function, chiropractors using EMG scans can diagnose stress patterns early. This makes surface EMG an essential tool for catching changes in nerve and muscle function—even before the patient feels a thing.
Why Do These Abnormal Patterns Appear?
The root cause of abnormal EMG patterns is rarely muscular—it’s neurological. The nerves that communicate with postural muscles are under constant influence from the brain and spinal cord. When this communication is altered by subluxation, environmental toxins, or nerve compression, the muscles respond accordingly.
For example:
- A nerve is compressed in the cervical region → upper trapezius overfires (hypertonicity).
- Early developmental interference from antibiotics → lumbar region underfires (hypotonicity).
- Chronic desk posture → full-spine asymmetry and increased energy output.
The RED model helps decode this. The “E” stands for Energy, which is exactly what surface EMG reflects. When energy usage is high, symmetry is low, and patterns are disorganized, the nervous system is expending more than it’s conserving. Over time, this depletes reserve and leads to dysfunction—even without pain.
That’s what happens if surface EMG is abnormal: the nervous system is waving a flag that it’s adapting inefficiently, and that it needs help before symptoms of nerve disorder or muscle disease surface.
How Chiropractors Use This Information to Shape Care Plans
Abnormal EMG patterns guide chiropractic care in a way no physical exam can match. With neuroCORE’s surface EMG technology, chiropractors build care plans based on real-time feedback from the nervous system—not just subjective symptoms.
- Hypertonic zones indicate overcompensation. Adjustments reduce neurological tension and restore tone balance.
- Hypotonic zones reveal disconnection. These areas need neural stimulation and stabilization.
- Asymmetrical patterns show spinal rotation, torsion, or energy waste. Adjustments re-establish coordinated nerve and muscle interaction.
Progress scans show reduced energy output, improved symmetry, and smoother tone patterns—signs that the nervous system is recalibrating. That’s how surface EMG provides proof your care is making a difference.
This isn’t about chasing dysfunction—it’s about restoring function. Chiropractors trained in neurological scanning aren’t reacting to symptoms—they’re responding to signals.
From Baseline to Breakthrough: The Power of Re-Scanning
When patients undergo EMG at multiple intervals, they provide the chiropractor with a window into neuroplastic change. INSiGHT’s scanning protocol includes:
- Initial Scan – Establishes the baseline.
- Progress Scan – Measures early change.
- Comparative Scan – Confirms neuroadaptive trends.
- Continuation Scan – Guides long-term wellness care.
Sometimes, a scan may look “worse” before it looks better—especially when patients undergoing EMG begin unwinding long-held patterns. This is not damage to nerves and muscles, but part of the adjustment process.
With this system, chiropractors can assess whether to increase or decrease frequency, modify adjustments, or address underlying nerve disorder traits more directly. The scan becomes the map—and the nervous system becomes the guide.
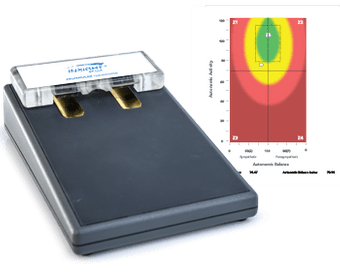
INSiGHT neuroCORE and the CORESCORE: Making the Invisible Visible
INSiGHT’s neuroCORE scanning system is a cornerstone of neurological analysis. With surface EMG, chiropractors gain a clear, reproducible view of spinal motor activity in less than 30 seconds.
- FDA-cleared Class II device
- Safe for children, pregnant patients, and the elderly
- Built for reproducibility with high inter-examiner reliability
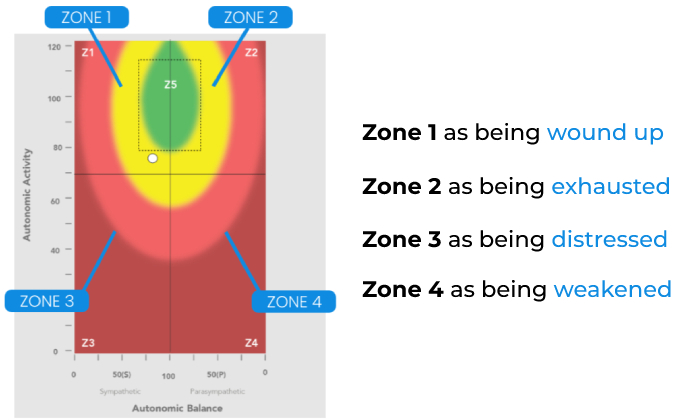
It also integrates with the CORESCORE, which combines:
- neuroCORE (sEMG)
- neuroTHERMAL (thermal differentials)
- neuroPULSE (HRV and autonomic tone)
This creates a three-dimensional analysis of neurological status, capturing both the electrical activity and adaptability of the nervous system. EMG is often used to diagnose inefficiencies in postural tone and reserve capacity—and when it’s part of CORESCORE, the data becomes more than visual. It becomes undeniable.
When Patterns Speak Louder Than Symptoms
In chiropractic, the most meaningful care doesn’t chase symptoms—it tracks performance. That’s why understanding what happens if surface EMG is abnormal is so essential. It shifts the focus from short-term relief to long-term neurological change.
Surface EMG shows you where energy is being spent, where coordination is breaking down, and where the nervous system is asking for attention. It does what no subjective exam can do: it records the electrical activity that powers posture and movement.
Whether you’re working with kids who’ve never had symptoms or adults stuck in years of sympathetic overdrive, abnormal EMG findings give you a place to start—and a path to follow.
Because when you can see the nervous system in motion, you stop adjusting in the dark. You adjust with purpose, precision, and proof.