One of the rites of passage every student of chiropractic must endure is learning a litany of eponymic orthopedic tests. Most of these tests are named for their developers. Therefore, instead of descriptive terms, students must memorize proper names which communicate nothing more than egomania. Proper names make great examination fodder. State boards love them. Until recently, few M.D.s or chiropractors questioned the validity of these procedures. Thankfully, this is changing.
A growing number of clinicians are beginning to question the appropriateness of orthopedic tests (1,2,3). Most of those which have been investigated have failed to demonstrate clinical utility. Walsh (4) recently wrote, “The use of orthopedic tests has been an integral part of the physical examination for a long time. They have remained a part of the examination more by virtue of common use than on the basis of any scientific demonstration of their validity and clinical significance. To make a judgement on the clinical worth of a test, its validity, reliability, sensitivity and specificity should ideally be known. Unfortunately, for most, if not all, orthopedic tests, these measures have not been determined.”
van den Hoogen et al (5) concluded, after a comprehensive literature review, that “Not one single test appeared to have high sensitivity and high specificity in radiculopathy.” For nonspecific low back pain, things are just as bad. Walsh (4) states, “The use of orthopedic tests in the valuation of non-specific LBP seems to be limited because of a generally low frequency of positive results and a lack of test validity.”
In sacroiliac joint dysfunction tests, Potter and Rothstein (6) found that “Reliability was poor.” Maigne et al (7) studied sacroiliac tests and concluded that “No pain provocation test reached statistical significance.”
What about stroke screening tests? After examining 12 patients with dizziness reproduced by extension-rotation and twenty healthy controls with Doppler ultrasound of the vertebral arteries, Cote et al (8) concluded, “We were unable to demonstrate that the extension-rotation test is a valid clinical screening procedure to detect decreased blood flow in the vertebral artery. The value of this test for screening patients at risk of stroke after cervical manipulation is questionable.” Terrett (9) noted, “There is also no evidence which suggests that positive tests have any correlation to future VBS (vertebrobasilar stroke) and SMT (spinal manipulative therapy).”
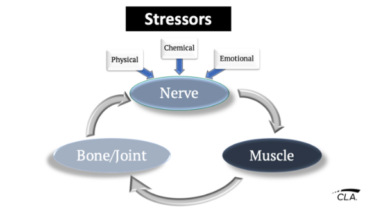
The lack of evidence for the stated purposes of these tests is bad enough. A more important question to ask is, “Do orthopedic tests reliably demonstrate the presence of vertebral subluxations?” I was unable to find any evidence to support the claim that they do.
One is compelled to ask, “If there is little to no evidence that these tests do what they were designed to do, and they do not provide useful information regarding vertebral subluxation, why do we embrace them?”
Colleges might reply, “Because they are asked on board exams.” Examiners might reply, “Because they are part of the core curriculum of all chiropractic colleges.”
With tongue firmly in cheek, an old psychology professor of mine wryly stated, “If you can’t measure something meaningful, measure something that’s easy to measure.” It is time to break this vicious cycle.
References
1. Souza T: “Which orthopedic tests are really necessary?” In: Lawrence DJ (ed): “Advances in Chiropractic. Volume 1.” Chicago. Mosby, 1994.
2. McCarthy KA: “Improving the clinician’s use of orthopedic testing: an application to low back pain.” Top Clin Chiropr 1994;1(1):42.
3. Deyo RA, Rainville J, Kent DL: “What can the history and physical examination tell us about low back pain? JAMA 1992;268(6):760.
4. Walsh MJ: “Evaluation of orthopedic testing of the low back for nonspecific lower back pain.” JMPT 1998;21(4):232.
5. van den Hoogen HM, Koes BW, van Eijk JT, Bouter LM: “On the accuracy of history, physical examination, and erythrocyte sedimentation rate in diagnosing low back pain in general practice.” Spine 1995;20(3):318.
6. Potter NA, Rothstein JM: “Intertester reliability for selected clinical tests of the sacroiliac joint.” Phys Ther 1985;65(11):1671.
7. Maigne JY, Aivaliklis A, Pfefer F: “Results of sacroiliac pain provocation tests in 54 patients with low back pain.” Spine 1996;21(16):1889.
8. Cote P, Kreitz B, Cassidy J, Thiel H: “The validity of the extension-rotation test as a clinical screening procedure before neck manipulation: a secondary analysis.” JMPT 1996;19:159.
9. Terrett AGJ: “Vertebrobasilar stroke following manipulation.” NCMIC, Des Moines, 1996. Page 32.