I regularly stand in front of chiropractic crowds and in the course of the conversation I ask, ‘What do you get paid for?’. The usual answers fly back.
‘Adjustments’ ‘Time spent’ ‘Outcomes’
All are partially correct but the real answer is that ‘you get paid to manage a care plan’.
Care Planning focuses on outcomes. Adjustments are part of the service and it takes time to observe and measure results. However, what we get paid for is our skill in creating and managing a patient’s specific care plan. That’s why it is so critically important that you get this right and adopt the latest and best proven strategies in planning the care for your patients.
I refer to this as the Paradigm Lost concept where there were two paths that could be taken with respect to care planning and neither of them are as relevant today:
- Bait and Switch: This people-pleasing approach focuses on developing a short term plan to address symptoms and along the way your intention is to tell them the bigger story about chiropractic being useful in their overall health. This usually ends up with a preventative check-in plan which can be referred to as a maintenance plan; sort of like scheduling an oil change.
- Sheeple: This pre-programmed and no fuss approach could also be referred to as the ‘3-2-1 and out the door’ plan. Somewhere along your journey, a coach or trusted advisor has offered a standardised plan that is to be delivered at the time of the Day 2 Report. It’s usually well scripted and is similar, if not the same, for all adult patients and slightly modified to a lesser number of visits for paediatric care. The goal is usually to get them into a ‘wellness program’ on a 1 x month frequency. The wellness portion isn’t based on real-time objective data and the front desk staff are constantly recalling missed appointments since there is no ongoing strategic plan being followed.
In these paradigms, re-exams, if done regularly, are usually limited to palpation, range of motion (ROM) testing and asking the question, ‘How do you feel?’ or ‘Does that still hurt?’ questions. In most cases, the outcome of updated reporting is for the patient to be offered a less frequent care plan as some sort of reward for making it this far and everyone seems happy … until the problem arises again, and again.
The neuroAGE of Chiropractic care planning has arrived
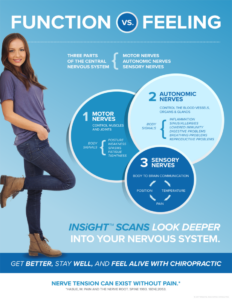
Care Planning, along with the timing and frequency of care delivery, need to be vastly different in today’s world. A paradigm shift has occurred as a result of the evolution of and increased use of instrument-based, functional neurological testing. These easy-to-use, objective tests create a new level of certainty for both the clinician and the patient. They force the communication and planning from symptom-based, feeling outcomes towards functional transformations. The shift has opened up the neuroAGE of chiropractic!
On the leading edge of this dynamic shift are the INSiGHT scanning technologies. These precision, neurological scanning devices are used exclusively to evaluate the impact of chiropractic adjustments as they are administered in a care plan. For over 30 years this technology has evolved within the profession so that the DNA of millions of chiropractic outcomes are built into the logic and engineering of every INSiGHT. This means that every exam and report in a monitored care plan brings to life the importance of remaining under watchful care while celebrating the amazing improvements in the functioning nervous system.

How does INSIGHT scanning make a difference in care planning?
The magic of chiropractic outcomes is based on adjusting the tone and tension within the spinal nervous system. Scanning the spine detects hidden patterns of autonomic and motor neurological distress when vertebral subluxations are present. Scanning the heart rate and rhythms provides a window into a patient’s adaptive response. The scope and relevance of these scans means that you can access neuroscience at your fingertips! Without looking deeply into the function of the central nervous system, chiropractors default to managing spinal and postural problems when the real issue lies deeper. You can’t get this data from X-rays and you can’t measure tension accurately by simply palpating, measuring Range Of Motion (ROM) or observing postures.