By Dr. Patrick Gentempo, Jr. and Dr. Christopher Kent
Chiropractic research has undergone a revolution in the last decade. Today, every chiropractic college has a formal department of research. Today, every chiropractic college has a formal department of research. The last few years have seen the establishment of chiropractic science journals and a growing number of scientific symposia.
Research is essential to the growth of chiropractic. Yet, our research resources are very limited, both in terms of dollars and talent. In our zeal to initiate research, it is important to keep several basic principles in mind.
Research to ‘prove’ chiropractic
Some factions within the profession feel we should concentrate our efforts on research projects to “prove what we already know is true — chiropractic works.” Of course, real research cannot be undertaken with such an objective in view. By its very nature, research seeks answers. One cannot “first draw the curve, then plot the points.” However, if we alter the objective a bit, research designs may exist to satisfy members of this faction.
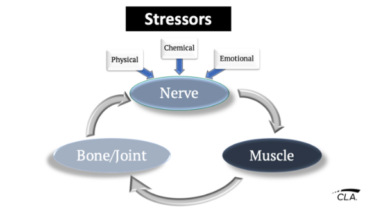
For example, we may pose questions concerning the effects of the vertebral subluxation complex on human health. Is there a difference in the rate of spinal degeneration in patients receiving chiropractic care vs. controls? Do chiropractic adjustments alter physiologic parameters? Which ones? Are long term changes produced in these parameters? Which techniques are most effective? To answer such questions, we must first determine how to detect and characterize vertebral subluxations.
Reliable and valid indicators of vertebral subluxation
Attempts to define vertebral subluxation bring to mind the words of a jurist in a pornography trial. In reference to pornography, the judge said, “I can’t define it, but I know it when I see it.”
Similarly, although vertebral subluxations are a part of the shared clinical experience of most practicing chiropractors, there is widespread disagreement concerning how subluxation should be defined. There is even more controversy concerning the criteria which should be applied in detecting and characterizing subluxations.
A positive move in the direction of defining vertebral subluxation was the establishment of the fivecomponent vertebral subluxation complex model. By defining the manifestations of subluxation in this fashion, we are in a position to determine what technologies may enable us to detect and quantify such phenomena.
The five components of the VSC as described by Flesia are: a. spinal kinesiopathology; b. neuropathology; c. myopathology; d. histopathology; e. pathology. Research to determine if reliable technologies exist to evaluate these components is a logical beginning. If not, the development of instruments and procedures to do so should be undertaken. Such research would immediately benefit the practitioner, particularly if such instruments and procedures were suitable for office use.
Happily, many such technologies exist. Unfortunately, their incorporation into chiropractic practice has been met with responses ranging from skepticism to outright hostility by the pseudoscientists who dominate the chiropractic research community.
The antitechnology movement is modern chiropractic
Contemporary chiropractic researchers have expressed the opinion that the reliability of diagnostic procedures should be established before they are introduced into general clinical practice. The authors heartily agree.
One question must necessarily follow: “How reliable is reliable enough?” The authors propose that “reliable enough” is “better than what most chiropractors are using.” Technologies are available right now to reliably monitor manifestations of spinal kinesiopathology, neuropathology, and myopathology. Some are relatively inexpensive.
These technologies have been developed outside the chiropractic profession. Studies have been published in refereed, peerreviewed science journals establishing their reliability (when properly used) and clinical utility. Yet certain chiropractic “scientists” reject them in favor of techniques exhibiting fairtopoor reliability.
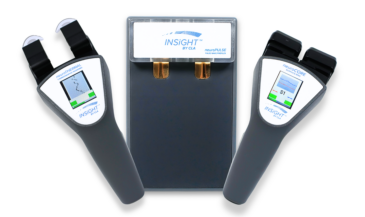
Consider two examples: paraspinal EMG scanning and videofluoroscopy. The reliability of surface electrode paraspinal EMG has been investigated at institutions including New York Chiropractic College [1]. The University of CaliforniaIrvine [2], and the Mayo Clinic [3]. Reliability coefficients ranging from 0.73 to 0.97 have been reported.
Further, a study by osteopaths found that paraspinal EMG activity decreased in patients (both symptomatic and asymptomatic) following spinal manipulation. Such changes were not seen in controls. [4]
Another study reported that “significant changes in muscle electrical activity occur as a consequence of adjusting.” [5] These findings have been published in refereed, peerreviewed journals. Paraspinal EMG scans have been accepted as evidence in courts of law.
In short, paraspinal EMG scanning has demonstrated an impressive level of reliability in studies conducted within and outside of the chiropractic profession. Studies have been published in scientific journals demonstrating changes following chiropractic adjustments and osteopathic manipulative therapy. The equipment is relatively inexpensive and very easy to use.
Videofluoroscopy is a technique that has been used in medicine for decades to evaluate pathomechanical changes in the cervical spine. Observational studies reported in refereed, peerreviewed medical journals have described cases where VF examinations revealed abnormalities not seen on traditional flexionextension studies. Some of these conditions were life threatening.
Modern VF equipment employs very low radiation levels. Substitution of one minute of fluoroscopy for the flexion and extension studies normally taken in a Davis series results in a radiation burden comparable to that of the traditional “plain films only” series. [6]
At least one chiropractic study concluded, “The current data indicate that VF determination of fixation in the cervical spine is a reliable procedure.” The examiners in the study achieved 84% agreement for the presence of fixation, 96% agreement for the absence of fixation, and 93% total agreement. [7]
In both instances, these technologies were developed by other professions and handed to us on a silver platter. As chiropractors, we had only to adapt the technology to our unique needs. Were these procedures embraced by the chiropractic research community? Certainly not!
Videofluoroscopy was declared “investigational” by the socalled “scientific affairs committee” of the American College of Chiropractic Radiology. Did they cite studies in the refereed literature to support their position? No! Did they conduct original research to support their position? No!
Similarly, the authors have received reports that some chiropractic “scientists” have been “trashing” surface EMG from the podium at license renewal seminars. They have allegedly declared it “unproven” and “not scientifically sound.” Interestingly, citations to support these pronouncements were conspicuously absent.
The alternatives
These “scientists” apply a far less burdensome standard to “low tech” methods of patient assessment. For example, few attack static or motion, palpation, although studies published in refereed journals indicate fairtopoor reliability. [8-12] The use of post-adjustment Xrays and VF have come “under the gun,” yet chiropractic “scientists” have been silent on the issue of the questionable sensitivity and specificity of plain film radiography for diagnostic purposes other than the characterization of subluxations.
Could it be that factors other than scientific detachment are operative here? Is the subliminal message that chiropractic should copy current medical “examinationers” in the study achieved 84% procedures, discarding those techniques which are uniquely chiropractic? Are chiropractic “scientists” concerned about preserving the “turf” of their DACCBR buddies? Do they look askance at any technology developed outside their circle?
Instead of using reliable measurements of physiologic phenomena generally accepted as being associated with the vertebral subluxation complex, many chiropractic “scientists” dance to the beat of a different drummer. Some chiropractic colleges and research organizations have engaged the services of clinical psychologists to design and direct chiropractic research projects. At least one has suggested the use of “paper and pencil” questionnaires as outcome criteria for therapeutic intervention. [13] In other words, the patient is asked to report subjective symptoms.
This should come as no surprise, since clinical psychologists generally lack training in the basic sciences of whole body anatomy, physiology, biochemistry, pathology and microbiology. Few psychologists are radiologists. Few are trained in wholebody physical examination procedures, or techniques of chiropractic analysis. There is nothing wrong with this, provided the psychologist is aware of such limitations.
Serious problems arise, however, when psychologists:
1. Eschew the value of basic science research in chiropractic.
2. Make pronouncements concerning the appropriateness of diagnostic studies they have not been trained to use.
3. Limit outcome assessment instruments to “paper and pencil” tests and subjective symptoms such as pain.
4. Employ the allopathic paradigm in research designs.
Manipulative mire
Another disturbing factor is the willingness of some chiropractic researchers to abandon chiropractic terminology as well as chiropractic analytic strategies. The generic moniker “spinal manipulation” or “spinal manipulative therapy” is becoming a replacement for the term “chiropractic adjustment.”
What’s wrong with that? They aren’t the same thing! There are techniques of chiropractic adjustment, such as basic, Grostic, etc., that simply do not fall under the medical definition of “manipulation.”
A grave error is also made in many studies of the effects of “manipulation” by lumping all “hands on” techniques together. What examination criteria are used to determine areas of subluxation (or “manipulable lesions,” to use the generic term)? Are they reliable? How do the investigators determine that the “manipulative treatment” was successful? Unreliable techniques like palpation? An audible release?
Would it not be absurd for medicine to test the efficacy of drug therapy for a given disease without defining the diagnostic criteria for the disease and specifying which drug is given and at which dosage? It is no less absurd to collectively refer to all chiropractic adjusting techniques as “manipulative treatments” without defining the technique used, the force applied, the direction of the force, and the criteria for pre and postadjusting analysis.
Research designs based upon “paper and pencil” questionnaires and the haphazard application of ill defined interventions based on unreliable criteria can hardly be considered “scientific.” As Huff observed in his book How To Lie With Statistics, “Permitting statistical treatment and the hypnotic presence of numbers and decimal points to befog causal relationships is little better than superstition…scantier evidence than this — treated in the statistical mill until common sense can no longer penetrate it — has made many a medical fortune and many a medical article in magazines, including professional ones.” [14]
The pain game
A number of chiropractors are also interested in research designs which compare the results of a diagnostic technology to patient symptomatology. The authors consider such efforts dubious at best.
For example, anatomical imaging modalities do not demonstrate pain. Some have criticized CT, MR, and fluoroscopic studies, claiming that many patients with reported abnormalities are asymptomatic. So what? CT, MR, and fluoroscopic studies simply demonstrate anatomy and pathologythey do not measure symptoms. How could any reasonable clinician expect them to? As has often been stated, “You can’t tell a living patient from a dead patient with an Xray.”
Similarly, physiologic monitoring devices such as paraspinal EMGs demonstrate functional changes. Does the instrument measure pain? Certainly not. It is a mystery to these authors why anyone would think otherwise. Why squander our limited resources on research which attempts to correlate these procedures with pain? If a doctor wants to quantitate a patient’s perception of pain, why not use the simple and inexpensive “paper and pencil” tests these researchers are so fond of?
Most proponents of these techniques have never claimed a correlation with pain. Our fear is that when it is “discovered” that these techniques do not correlate well with pain, such findings will be used in an attempt to discredit their utility.
We propose that many wellmeaning chiropractic researchers are putting the cart before the horse, and employing designs which are inherently flawed. In other instances, the research proposed is clearly designed to sell chiropractic care as a symptomatic treatment for musculoskeletal pain.
Chiropractic is not a subset of medicine. Chiropractic is concerned with the detection and correction of vertebral subluxations. The courts and legislatures have, with few exceptions, maintained that chiropractic is not medicine, but is a separate and distinct science. As such, it has different objectives which necessitate different outcome assessments.
Chiropractic and medicine share the objective of promoting human health. Their respective strategies for doing so, however, are radically different.
Electricians don’t fix leaky faucets. The disappearance of leaks (or someone’s perception that a leak has disappeared) is certainly not a reasonable outcome assessment for the work of an electrician. Would it not be absurd to apply the same rules to basketball as those applied to football, claiming that both were subsets of the broader category “ball games?”
Some might argue that research is research, and that the same designs may be used by all scientists. That is precisely the point. As they say in the computer world, “garbage ingarbage out.” Competent research designs are dependent upon an understanding of the basic sciences, a working knowledge of understanding of the basic sciences, a working knowledge of contemporary analytic procedures, and an understanding of chiropractic philosophy.
Appropriate outcome assessments must be employed, based upon an understanding of what the objectives of chiropractic care are. Interventions must be clearly defined. Criteria for the successful (or unsuccessful) application of an intervention must be defined. What fruit has been borne by the allopathic research programs currently underway? The aberrant perception by students and some chiropractors that chiropractic is a subset of medicine, and that adjusting is a subset of manipulation? The perception that chiropractic care is temporary analgesia at best, and placebo therapy at worst?
Consider the following:
XXX INSERT TABLE XXX
What should we expect from chiropractic research? The authors propose the following:
A. Improved understanding of the effects of the vertebral subluxation on human health.
B. Reliable and valid technologies for detecting, characterizing, and correcting vertebral subluxations.
C. Information concerning the relative effects of different adjusting techniques on specific outcome criteria.
D. Improved techniques of spinal analysis and adjusting. The value of chiropractic research lies in its ability to improve our clinical strategies, and to provide us with a scientifically sound basis for making claims to the public and the scientific community.
“Paradigmosis” is a disorder characterized by faulty research designs leading to erroneous conclusions. The etiology is a lack of understanding of the basic sciences, clinical sciences, and philosophy of chiropractic. The principal symptom is the use of symptoms as outcome criteria. The condition, while not fatal, may be crippling to the profession afflicted with it.
References
1. Spector B: “Surface electromyography as a model for the development of standardized procedures and reliability testing.” JMPT 2(4):214, 1979.
2. Cram J: “Clinical EMG: Muscle Scanning for Surface Recordings.” Biofeedback Institute of Seattle. Seattle, WA, 1986.
3. Thompson J, Erickson R, Offord K: “EMG muscle scanning: stability of hand held electrodes.” Biofeedback Self Regul 14(1):55,1989.
4. Ellestad S, Nagle R, Boesler D, Kilmore M: “Electromyographic and skin resistance responses to osteopathic manipulative treatment for low back pain.” JAOA 88(8):991, 1988.
5. Shambaugh P: “Changes in electrical activity in muscles resulting from chiropractic adjustment: a pilot study.” JMPT 10(6):300, 1987.
6. Kent C: “The role of videofluoroscopy in chiropractic practice.” ICA Review 46(1):41, 1990.
7. Antos J, Robinson GK, Keating JC, Jacobs GE: “Interexaminer reliability of cinefluoroscopic detection of fixation in the midcervical spine.” Proceedings of the Scientific Symposium on Spinal Biomechanics, International Chiropractors Association, 1989.
8. Keating J: “Interexaminer reliability of motion palpation of the lumbar spine: a review of the quantitative literature.” Proceedings of the Scientific Symposium on Spinal Biomechanics, International Chiropractors Association, 1989.
9. Cassidy J, Potter G: “Motion palpation of the lumbar spine.” JMPT 2(3):151, 1979.
10. Gonella C, Paris S, Kutner S: “Reliability in evaluating passive intervertebral motion.” Phys Ther 62(4):436, 1982.
11. Juli G, Bullock M: “A motion profile of the lumbar spine in an agine population assessed by manual examination.” Physiotherapy Practice 3:70, 1982.
12. Boline P, Keating J, Brist J, Denver G: “Interexaminer reliability of palpatory examinations of the lumbar spine.” Am J Chiro Med 1(1):5, 1988.
13. Jansen RD: “Professional success: Measuring outcomes, not incomes.” Dynamic Chiropractic 8(9):35, 1990.
14. Huff D: “How to Lie With Statistics,” W.W. Norton, New York, NY, 1954.